File
advertisement

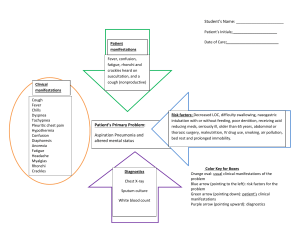
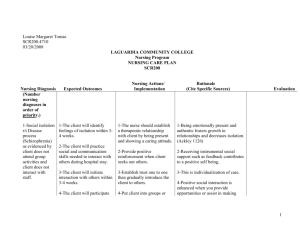
CRITICAL THINKING SUMMARY Student: _Heather Hulien_ Client Dx: __COPD exacerbation, Bronchitis_ Age: _58_ Allergies: __No known allergies_ The MEDICAL DIAGNOSIS that brought the client to the hospital is: COPD exacerbation, bronchitis PATHOPHYSIOLOGY of diagnosed disease: (From text) Chronic bronchitis is defined as hypersecretion of mucus and chronic productive cough for at least 3 months of the year for at least 2 consecutive years. Inspired irritants result in airway infiltration of neutrophils, macrophages, and lymphocytes into the bronchial wall. Continual bronchial inflammation causes bronchial edema and increases the size and number of mucous glands and goblet cells in the airway epithelium. Thick, tenacious mucous is produced and cannot be cleared because ciliary function is impaired (Huether & McCance, 2012). SYMPTOMS typically seen with this diagnosis include (as identified in your text): Productive cough, dyspnea, wheezing, history of smoking, barrel chest, prolonged expiration, cyanosis, chronic hypoventilation, polycythemia, and Cor pulmonale (Huether & McCance, 2012). CLIENT’S SYMPTOMS of the diagnosed disease include: Increasing dyspnea, an increase in her chronic cough (no sputum production), shortness of breath, and wheezing. NUTRITIONAL ASSESSMENT: Height (actual or estimated): _165 cm_ Weight (actual or estimated): _55.7 kg_ Estimate Ideal Body Weight (Male: 105lb + 6 lb/inch > 5’. Female: 100lb + 5lb/inch > 5’): 125 Pounds_ Does this client have characteristics of a well-nourished person? Yes _____ No __X__ Explain your answer. The patient does not exclusively have characteristics of a well-nourished person. Although the patient appears to eat foods from all five food groups, has shiny hair, white teeth, a healthy skin tone, strong fingernails, and normal protein and albumin levels, she easily becomes fatigued with activity, and she lacks energy. She is unable to finish many of her meals because she does not have enough energy. The patient stated that she has recently lost five pounds. PSYCHOSOCIAL STAGE OF DEVELOPMENT What is the client’s developmental stage? The patient is in the stage of generativity versus stagnation (middle adulthood) (Taylor, Lillis, LeMone, & Lynn, 2011). Has he/she met the necessary accomplishments? Yes __X__ No _____ Explain. The patient is involved with her children and grandchildren. She also interacts with her community by attending church and many church events. Although she is not currently working, she worked for several years in the food service industry. How is this illness affecting the client’s ability to meet these necessary accomplishments? Since the patient is in the hospital, she is not able to care for her children and grandchildren. She is also unable to attend several church events that she had been looking forward to attending. She recently had to quit working because her lack of energy and shortness of breath made her physically demanding job too difficult to complete. NURSING DIAGNOSIS/OBJECTIVES/INTERVENTIONS Indicate below the 2 priority nursing diagnoses that are most relevant for your client. #1 NURSING DIAGNOSIS (problem r/t) Risk for ineffective airway clearance related to bronchoconstriction, increased sputum production, ineffective cough, and fatigue/ lack of energy (Ladwig & Ackley, 2011). DEFINING CHARACTERISTICS (S/S) that support this diagnosis: Absent cough; adventitious breath sounds; changes in respiratory rate and rhythm; cyanosis; difficulty vocalizing; diminished breath sounds; dyspnea; excessive sputum; orthopnea; restlessness; wide-eyed (Ladwig & Ackley, 2011). OBJECTIVE/CLIENT OUTCOME for this diagnosis: The patient will maintain a patent airway at all times during her stay in the hospital. NURSING INTERVENTIONS that will assist the client to resolve the above identified diagnosis: 1. Teach the client to deep breathe and perform controlled coughing (Ladwig & Ackley, 2011). 2. Teach the client the proper technique for using an incentive spirometer (Ladwig & Ackley, 2011). 3. Administer medications such as bronchodilators or inhaled steroids as ordered (Ladwig & Ackley, 2011). #2 NURSING DIAGNOSIS (problem r/t) Ineffective breathing pattern related to shortness of breath, mucus, bronchoconstriction, and airway irritants (Ladwig & Ackley, 2011). DEFINING CHARACTERISTICS (S/S) that support this diagnosis: Alterations in depth of breathing; altered chest excursion; assumption of three-point position; bradypnea; decreased minute ventilation; decreased vital capacity; dyspnea; increased anterior-posterior diameter; nasal flaring; orthopnea; prolonged expiration phase; pursed-lip breathing; tachypnea; use of accessory muscles to breathe (Ladwig & Ackley, 2011). OBJECTIVE/CLIENT OUTCOME for this diagnosis: The patient will demonstrate a breathing pattern that supports blood gas results within the client’s normal parameters during her stay in the hospital. NURSING INTERVENTIONS that will assist the client to resolve the above identified diagnosis: 1. Teach the patient to use pursed-lip and controlled breathing techniques (Ladwig & Ackley, 2011). 2. Coach the client to slow respiratory rate (Ladwig & Ackley, 2011). 3. During hyperventilation, instruct the patient to breathe in and out of a paper bag as tolerated (Ladwig & Ackley, 2011). COMPLICATIONS: If this client’s condition were to worsen, what would be the most likely reason and why? If the patient’s condition were to worsen, the most likely reason would be respiratory alkalosis due to ineffective breathing. When breathing becomes labored, the body’s reaction is to breathe faster. Fast breathing causes the body to blow off carbon dioxide and leads to abnormally low levels of carbon dioxide in the blood. How would you know this is happening? The nurse would know this is happening because the patient could experience dizziness, confusion, tingling of extremities, convulsions, and coma. What will you do if this happens? If this happens, the nurse would encourage the patient to slow respiratory rate and notify the physician immediately. The nurse would expect an order for arterial blood gases. PHYSICIAN PRESCRIBED MEDICATIONS AND INTERVENTIONS MEDS/IVs/TX/DIET (Include dose, route, frequency) REASON PRESCRIBED (Drug Classification, What is it treating?) Albuterol: 5mg; NEB; every 4 hours Bronchodilators/ adrenergics; used to control and prevent reversible airway obstruction caused by COPD Ipratropium: 0.5 mg; NEB; ever 4 hours Bronchodilators/ anticholinergics; maintenance therapy of reversible airway obstruction due to COPD Rifampin; 300 mg; PO; every Monday, Wednesday, and Friday Antituberculars; active tuberculosis ethambutol: 800 mg; PO; every Monday, Wednesday, and Friday Antituberculars; active tuberculosis NURSING IMPLICATIONS FROM TEXT (Checking for adverse reactions, preparation & administration concerns) Shake inhaler well, and allow at least 1 minute between inhalations Administer adrenergic bronchodilators first, followed by ipratropium, the corticosteroids. Wait 5 minutes between medications; solution for nebulization can be diluted with preservative-free 0.9% NaCl Administer medication on an empty stomach at least 1 hour before or 2 hours after meals with a full glass of water Given as a single daily dose; should be given at the same time each day; administer with food or milk to minimize GI irritation; tablets may be crushed and mixed with apple juice or apple sauce CLIENT DATA FROM YOUR ASSESSMENT (What data is important to know before & after giving) Assess lung sounds, pulse, and BP before administration and during peak of medication. Note amount, color, and character of sputum produced; monitor pulmonary function tests before initiating therapy and periodically during therapy; observe for paradoxical bronchospasm (wheezing); may cause transient decrease in serum potassium concentrations Assess for allergy to atropine and belladonna alkaloids; assess respiratory status before administration and at peak of medication Mycobacterial studies and susceptibility tests should be performed before and periodically during therapy to detect possible resistance; assess lung sounds and character and amount of sputum periodically during therapy; evaluate renal function, CBC, and urinalysis periodically and during therapy Mycobacterial studies and susceptibility tests should be performed before and periodically during therapy to detect possible resistance; assess lung sounds and character and amount of sputum periodically during therapy; assessments of visual function should be made frequently during therapy; montelukast: 10 mg; PO; every night Bronchodilator/ leukotriene antagonists; prevention of bronchoconstriction Administer once daily in the evening; assess for rash during therapy; monitor closely for changed in behavior that could indicate the emergence or worsening of depression or suicidal thoughts Alprazolam: 0.5 mg; PO; three times a day PRN Antianxiety agents/benzodiazepines; anxiety associated with depression Administer with food if GI upset occurs; administer greatest dose at bedtime to avoid daytime sedation Furosemide: 20 mg, PO, twice a day PRN Diuretics/ loop diuretics: edema Give last dose no later than 5 pm to minimize disruption of sleep cycle; may be given with food or milk to minimize gastric irritation; tablets may be crushed (Vallerand, Sanoski & Deglin, 2014) monitor renal and hepatic functions, CBC, and uric acid levels Assess lung sounds and respiratory function prior to and periodically during therapy; assess allergy symptoms before and periodically during therapy; may cause an increase in AST and ALT concentrations Assess degree and manifestations of anxiety and mental status prior to and periodically during therapy; assess patient for drowsiness, lightheadedness, and dizziness; assess CNS effects and risk of falls; monitor CBC and liver and renal function periodically during longterm therapy; may cause decreased hematocrit and neutropenia Assess fluid status; monitor daily weight, intake and output ratios, amount and location of edema, lung sounds, skin turgor, and mucous membranes; monitor BP and pulse before and during administration; assess patient for tinnitus and hearing loss; assess for allergies to sulfonamides; assess patient for skin rash during therapy; monitor electrolytes renal and hepatic function, serum glucose, and uric acid levels before and periodically throughout therapy Analysis of Diagnostic Tests DIRECTIONS: 1. List all diagnostic and laboratory tests pertinent to the patient's medical diagnosis or medical treatments (i.e. medications) and provide the patient values for each test. Explain why they are pertinent for this patient. 2. List any screening diagnostic and laboratory tests that are not within normal limits. Explain why these tests are increased or decreased in relation to your patient's medical condition. Diagnostic/Lab Test Chest X ray Glucose Patient Values Lungs are mildly hyperextended; mild diffuse interstitial coarsening 122 High ALT Neut Auto 48 High 87.4 High Lymph auto Lymph absolute 8.5 low 0.67 Low (Van Leeuwen, Poelhuis-Leth & Bladh, 2013) Analysis of Values COPD Could indicate impaired fasting glucose Could indicate liver damage Could be a result of tuberculosis; could indicate acute infection or acute stress Could be a result of steroid use Could be a result of steroid use References Huether, S.E., & McCance, K.L. (2012). Understanding pathophysiology. (5th ed., p. 114-693). Elsevier Inc. Ladwig, G.B., & Ackley, B.J. (2011). Mosby’s guide to nursing diagnosis. (3rd ed.). Maryland Heights, MO: Mosby Elsevier Taylor, C.R., Lillis, C., LeMone, P., & Lynn, P. (2011). Fundamentals of nursing: The art and science of nursing care. (7th ed., p. 366). Philadelphia, PA: Lippincott Williams & Wilkins. Vallerand, A.H., Sanoski, C.A., & Deglin, J.H. (2014). Davis’s drug guide for nurses. (13th ed.). Unbound Medicine, Inc. Van Leeuwen, A.M., Poelhuis-Leth, D.J., & Bladh, M.L. (2013). Davis’s comprehensive handbook of laboratory and diagnostic tests with nursing implications. Unbound Medicine, Inc.