Aspiration Pneumonia Care Plan: Nursing Interventions & Goals
advertisement

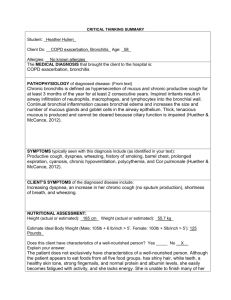
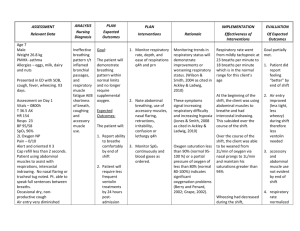
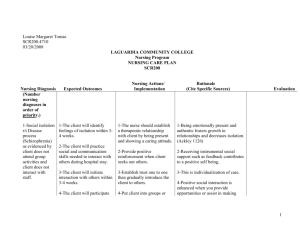
Student’s Name: _____________________ Patient’s Initials: _____________________ Patient manifestations Clinical manifestations Cough Fever Chills Dyspnea Tachypnea Pleuritic chest pain Hypothermia Confusion Diaphoresis Anorexia Fatigue Headache Myalgias Rhonchi Crackles Date of Care:_________________________ Fever, confusion, fatigue, rhonchi and crackles heard on auscultation, and a cough (nonproductive) Patient’s Primary Problem: Aspiration Pneumonia and altered mental status Diagnostics Chest X-ray Sputum culture White blood count Risk factors: Decreased LOC, difficulty swallowing, nasogastric intubation with or without feeding, poor dentition, receiving acid reducing meds, seriously ill, older than 65 years, abdominal or thoracic surgery, malnutrition, IV drug use, smoking, air pollution, bed rest and prolonged immobility. Color Key for Boxes Orange oval: usual clinical manifestations of the problem Blue arrow (pointing to the left): risk factors for the problem Green arrow (pointing down): patient’s clinical manifestations Purple arrow (pointing upward): diagnostics Patient Problem #1: Ineffective airway clearance Short term Goal: The patient will demonstrate effective coughing and clear breath sounds within two days. Long term Goal: The patient will maintain a patent airway at all times throughout hospital stay 5 Nursing Interventions (put rationales in parentheses right after each intervention with appropriately cited reference): 1. Position the client to optimize respiration (e.g. head of bed elevated 30 to 45 degrees). (An upright position allows for maximal lung expansion; lying flat causes abdominal organs to shift toward the chest, which crowds the lungs and makes it more difficult to breathe) (Ackley, Ladwig, Makic, page 130-132) 2. Help the client deep breathe and perform controlled coughing. (Controlled coughing uses the diaphragmatic muscles, making the cough more forceful and effective.) (Ackley, Ladwig, Makic, page 130-132) 3. Encourage activity and ambulation as tolerated. If the client cannot be ambulated, turn the client from side to side at least every 2 hours. (Body movement helps mobilize secretions) (Ackley, Ladwig, Makic, page 130-132) 4. Observe sputum noting color, odor, and volume. (Normal sputum is clear or grey and minimal; abnormal sputum is green, yellow, or bloody; malodorous; and often copious.) (Ackley, Ladwig, Makic, page 130-132) 5. Administer bronchodilators as ordered to assist with airway patency. (Bronchodilators relieve bronchospasm, reduce airway obstruction, and aid in secretion clearance) (Honan, p.349) 6. If not contraindicated by patient’s cardiac status, encourage fluids to 2500mL/day. (Keeping the patient well hydrated helps thin respiratory secretions and makes them easier to expectorate.) (Ackley, Ladwig, Makic, page 130-132) Outcome (Evaluation) How will you know that patient achieved the goals?: Short term goal met, patient had productive cough and clear breath sounds. Long term goal not met, cannot evaluate until patient is discharged. Patient Problem #2: Risk for aspiration r/t impaired ability to swallow Short term Goal: Pt. will have no episodes of aspiration for 2 days. Long term Goal: Pt. will digest gastric feeding without aspiration within the next two weeks. 5 Nursing Interventions (put rationales in parentheses right after each intervention with appropriately cited reference): 1.Monitor respiratory rate, depth, and effort. Note any signs of aspiration such as dyspnea, cough, cyanosis, wheezing, hoarseness, foul smelling sputum, or fever. If new onsets of symptoms, perform oral suction and notify provider immediately. (Signs of aspiration should be detected as soon as possible to prevent further aspiration and to initiate treatment that can be lifesaving.) (Ackley, Ladwig, Makic, page 147-148) 2.Assess the abdomen and listen to bowel sounds frequently, noting if they are decreased, absent, or hyperactive. (Decreased or absent bowel sounds can indicate an ileus with possible vomiting and aspiration; increased high pitched bowel sounds can indicate a mechanical bowel obstruction with possible vomiting and aspiration.) (Ackley, Ladwig, Makic, page 147-148) 3.Note new onset of abdominal distention or increased rigidity of abdomen. (Abdominal distention or rigidity can be associated with paralytic or mechanical obstruction and an increased likelihood of vomiting and aspiration) (Ackley, Ladwig, Makic, page 147-148) 4.Provide meticulous oral care including brushing of teeth at least 2 times per day. (Good oral care can prevent bacterial or fungal contamination of the mouth, which can be aspirated.) (Ackley, Ladwig, Makic, page 147-148) 5.Minimize the use of sedatives and other medications that decrease level of consciousness. (Sedation agents can reduce cough and gag reflexes as well as interfere with the clients’ ability to manage oropharyngeal secretions.) (Ackley, Ladwig, Makic, page 147-148) Outcome (Evaluation) How will you know that patient achieved the goals?: Short term goal met; there have been no episodes for the last 2 days. Long term goal not met, patient was not able to digest gastric feeding without aspiration. Patient Problem #3: Risk for falls related to lower extremity weakness Short term Goal: Patient will remain free of falls for 2 days. Long term Goal: Patient will identify factors that increase potential for injury by the end of the week. 5 Nursing Interventions (put rationales in parentheses right after each intervention with appropriately cited reference): 1. Carefully assist a mostly immobile patient up. Be sure to lock the bed and wheelchair and have sufficient personnel to protect the client from falls. When rising from a lying position, have the client change positions slowly, dangle legs, and stand next to the bed before walking to prevent orthostatic hypotension. (Encourage client engagement in a monitored exercise program that will strengthen core and lower extremities to reduce fall risk.) (Ackley, Ladwig, Makic, page 355-357) 2. 3. Use a “high risk fall” armband/bracelet and fall risk room sign to alert staff for increased vigilance and mobility assistance. (These steps alert the nursing staff of the increased risk for falls.) (Ackley, Ladwig, Makic, page 355-357) Place a fall prone client in a room that is near the nurse’s station. (Such placement allows more frequent observation of the client.) (Ackley, Ladwig, Makic, page 355-357) 4. Help clients sit in a stable chair with arm rests. Avoid use of wheelchairs except for transportation as needed. (Clients are likely to fall when in a wheelchair because they may stand up without locking the wheels or removing the foot rests. Wheelchairs do not increase mobility; people just sit in them the majority of the time.) (Ackley, Ladwig, Makic, page 355-357) 5. Refer to physical therapy or other programs for exercise programs that target strength, balance, flexibility, or endurance. (Programs with at least two of these components have been shown to decrease the rate of falling and number of people falling.) (Ackley, Ladwig, Makic, page 355-357) Outcome (Evaluation) How will you know that patient achieved the goals?: Short term goal met, patient has not had any falls. Long term goal is still in progress. References Ackley, B., Ladwig, G., & Makic, M. (2017) Nursing diagnosis handbook: an evidence-based guide to planning care. (11th ed.) St. Louis: Elsevier. Honan, L. 2019. Focus on adult health: Medical-surgical nursing. Philadelphia: Wolters Kluwer.