Perinatal Asphyxia
advertisement
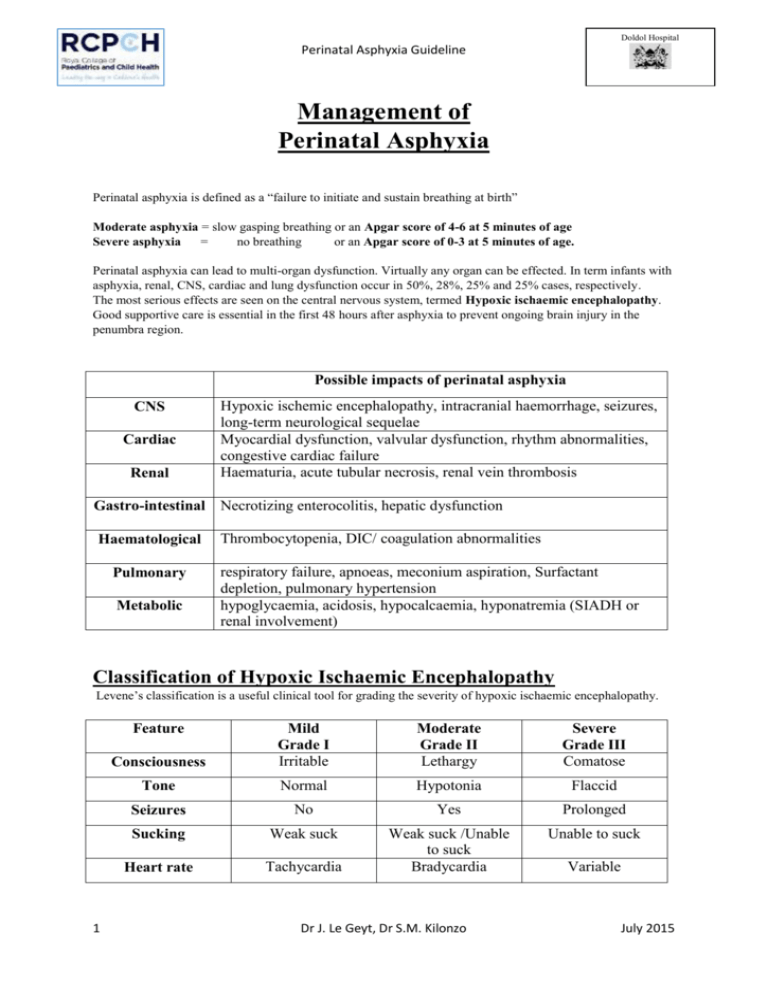
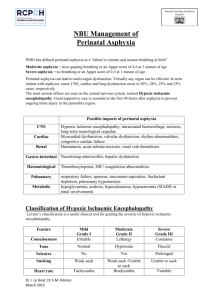
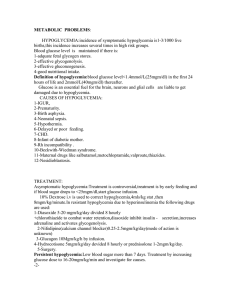
Doldol Hospital Perinatal Asphyxia Guideline Management of Perinatal Asphyxia Perinatal asphyxia is defined as a “failure to initiate and sustain breathing at birth” Moderate asphyxia = slow gasping breathing or an Apgar score of 4-6 at 5 minutes of age Severe asphyxia = no breathing or an Apgar score of 0-3 at 5 minutes of age. Perinatal asphyxia can lead to multi-organ dysfunction. Virtually any organ can be effected. In term infants with asphyxia, renal, CNS, cardiac and lung dysfunction occur in 50%, 28%, 25% and 25% cases, respectively. The most serious effects are seen on the central nervous system, termed Hypoxic ischaemic encephalopathy. Good supportive care is essential in the first 48 hours after asphyxia to prevent ongoing brain injury in the penumbra region. Possible impacts of perinatal asphyxia CNS Cardiac Renal Hypoxic ischemic encephalopathy, intracranial haemorrhage, seizures, long-term neurological sequelae Myocardial dysfunction, valvular dysfunction, rhythm abnormalities, congestive cardiac failure Haematuria, acute tubular necrosis, renal vein thrombosis Gastro-intestinal Necrotizing enterocolitis, hepatic dysfunction Haematological Pulmonary Metabolic Thrombocytopenia, DIC/ coagulation abnormalities respiratory failure, apnoeas, meconium aspiration, Surfactant depletion, pulmonary hypertension hypoglycaemia, acidosis, hypocalcaemia, hyponatremia (SIADH or renal involvement) Classification of Hypoxic Ischaemic Encephalopathy Levene’s classification is a useful clinical tool for grading the severity of hypoxic ischaemic encephalopathy. Feature 1 Consciousness Mild Grade I Irritable Moderate Grade II Lethargy Severe Grade III Comatose Tone Normal Hypotonia Flaccid Seizures No Yes Prolonged Sucking Weak suck Unable to suck Heart rate Tachycardia Weak suck /Unable to suck Bradycardia Dr J. Le Geyt, Dr S.M. Kilonzo Variable July 2015 Doldol Hospital Perinatal Asphyxia Guideline Management post resuscitation; All babies of moderate or severe perinatal asphyxia should be transferred to a newborn unit for minimum 48 hours. If the clinical course is not typical of a hypoxic-ischaemic insult, consider other causes (possible other causes include [but are not limited to] metabolic disease, infection, drug exposure, CNS malformation, or neonatal stroke) Temperature control - Avoid hypothermia or hyperthermia Check vital signs - Fluids - All babies with moderate or severe perinatal asphyxia should be started on intravenous Immediate clinical assessment, recording respiration, heart rate, blood pressure, capillary refill time, temperature and oxygen saturation. maintenance fluids. - Urine output monitoring (consider catheterisation) - If low urine output, oedema, or significant renal impairment in the UECs, fluid restrict to 2/3rd maintenance. Feeding - All babies with severe perinatal asphyxia, or clinical signs of HIE grade II, should be kept nil by mouth for the first 48 hours - All babies with moderate perinatal asphyxia, or clinical signs of HIE grade I, should be kept nil by mouth for the first 24 hours - If inadequate suck, feed by NG tube - If frequent seizures, apnoeas, respiratory distress, or evidence of NEC or GI bleeding, remain nil by mouth. Investigations – Blood sugar at admission, then twice daily - FHG, UECs, LFTs at 24 hours (unless clinically indicated earlier eg pallor, jaundice) Seizures – First line treatment is phenobarbitone (20 mg/kg) unless significant apnoeas or respiratory depression is present. If there is no response, two additional doses of 10 mg/kg can be given 2 - If convulsions are still uncontrolled, phenytoin sodium should be added (20mg/kg) - Maintenance therapy of both phenobarbitone and phenytoin is started 12 hours later at a dose of 5 mg/kg/day in a single dose. - Anticonvulsants can be stopped after 48 hours without seizures (unless the baby has been on them for >7days, then wean over 3 days) Neurological examination - Assessment twice daily Dr J. Le Geyt, Dr S.M. Kilonzo July 2015 Doldol Hospital Perinatal Asphyxia Guideline Prognosis Neurodevelopmental outcome correlates closely with the severity of HIE (it does not correlate well to Apgar scores). The baby’s diagnosis should be its worst HIE grade during admission. HIE grade I HIE grade II HIE grade III ; <2% have any long term neurological complications ; 30-50% die or have long term neurological complications ; 70-80% die or have severe long term neurological complications, 10% have moderate long term neurological complications Grade I HIE do not require routine neuro-developmental follow-up. Grade II and III should have neuro-developmental assessments (and intervention if needed) at follow-up clinics for at least the first 18 months of life. References 3 “The Apgar Score”. American Committee on Obstetrics Practice Fetus and Newborn / American Academy of Pediatrics, Committee Opinion. 2010. “Post-resuscitation management of asphyxiated neonates”. R. Agarwal, et al. Division of Neonatology, All India Institute of Medical Sciences, New Delhi, India. WHO Collaboration Centre. 2007 Dr J. Le Geyt, Dr S.M. Kilonzo July 2015