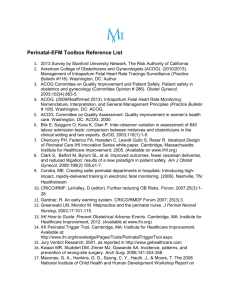
Perinatal Deep Dive Structure Tool
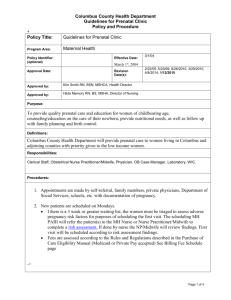
advertisement
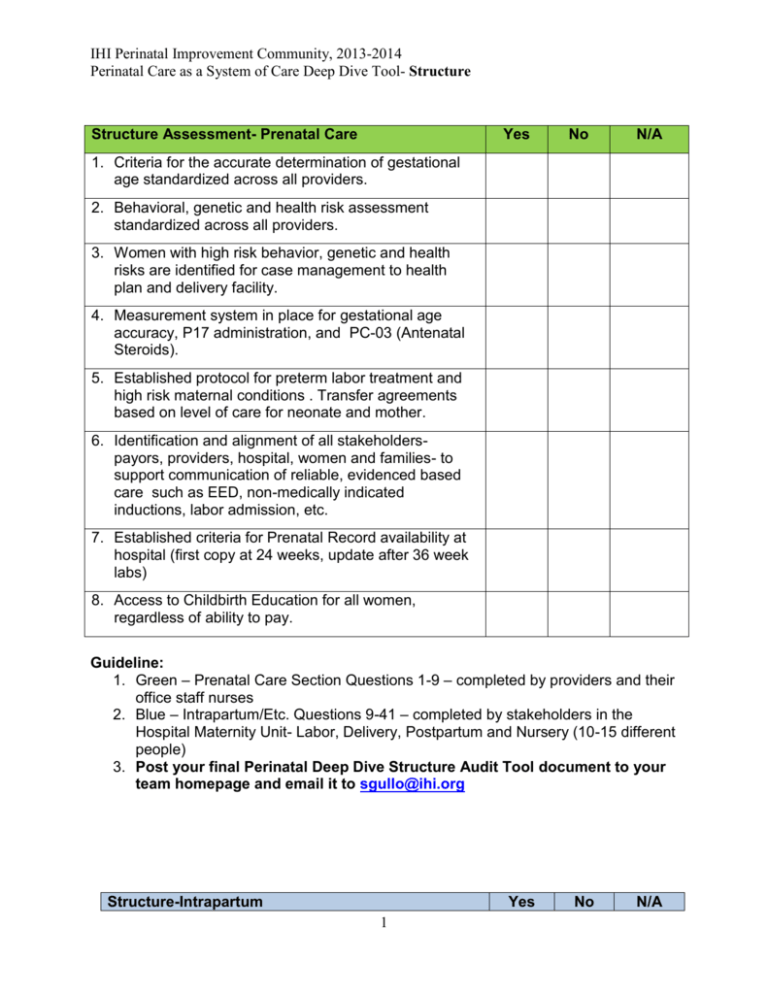
IHI Perinatal Improvement Community, 2013-2014
Perinatal Care as a System of Care Deep Dive Tool- Structure
Structure Assessment- Prenatal Care
Yes
No
N/A
1. Criteria for the accurate determination of gestational
age standardized across all providers.
2. Behavioral, genetic and health risk assessment
standardized across all providers.
3. Women with high risk behavior, genetic and health
risks are identified for case management to health
plan and delivery facility.
4. Measurement system in place for gestational age
accuracy, P17 administration, and PC-03 (Antenatal
Steroids).
5. Established protocol for preterm labor treatment and
high risk maternal conditions . Transfer agreements
based on level of care for neonate and mother.
6. Identification and alignment of all stakeholderspayors, providers, hospital, women and families- to
support communication of reliable, evidenced based
care such as EED, non-medically indicated
inductions, labor admission, etc.
7. Established criteria for Prenatal Record availability at
hospital (first copy at 24 weeks, update after 36 week
labs)
8. Access to Childbirth Education for all women,
regardless of ability to pay.
Guideline:
1. Green – Prenatal Care Section Questions 1-9 – completed by providers and their
office staff nurses
2. Blue – Intrapartum/Etc. Questions 9-41 – completed by stakeholders in the
Hospital Maternity Unit- Labor, Delivery, Postpartum and Nursery (10-15 different
people)
3. Post your final Perinatal Deep Dive Structure Audit Tool document to your
team homepage and email it to sgullo@ihi.org
Structure-Intrapartum
Yes
1
No
N/A
IHI Perinatal Improvement Community, 2013-2014
Perinatal Care as a System of Care Deep Dive Tool- Structure
9. Gestational age criteria standardized and validated
on admission.
10. Prenatal record available at admission- on unit or
with the mother.
11. Consistent handoff tool {SBAR, etc} specify tool
used
12. Bedside rounds with care team- patient perspective
“nothing about me without me”.
13. RN empowered to call neonatal team
14. RN empowered to call cesarean team (not to
diagnose the need for cesarean, but to activate the
team)
15. Individual Provider data published – start with
Perinatal Core Measures*
16. Established team huddle and communication with
patient/family at critical decision points in the patient
journey. Example- (1)admission, (2)when patient is
complete to review risk factors to proceed forward,
(3)other examples- after 2 hours with minimal or no
progress, discuss plan of care to include- forceps,
vacuum, CB, continuation of pushing, etc.)
Fetal Monitoring Structure
17. Multidisciplinary Fetal Monitoring Education core
component of obstetrical provider and nursing
credentialing.
18. Fetal monitoring documentation tools are consistent
with NICHD terminology- paper or electronic.
19. Clinical algorithm for management of
indeterminate/abnormal FHR patterns (NICHD 2009)
in place.
20. Established multidisciplinary EFM strip and case
reviews.
High Risk Medications
21. Standard mixture and policy for oxytocin and other
high risk medications
22. If provider opts out of standard order set, system in
place to identify and address when standardized
dosage is not followed.
23. Team definition for tachysystole and established
clinical algorithm for identification and management
of tachysystole.
24. Informed Consent for oxytocin administrationinduction and augmentation.
Structure-Intrapartum
Yes
2
No
N/A
IHI Perinatal Improvement Community, 2013-2014
Perinatal Care as a System of Care Deep Dive Tool- Structure
Labor Management
25. Team definition for admission criteria
26. Team definition for labor
27. Definition and criteria for labor augmentation
28. Established pain management plan for all stages of
labor, including latent phase
29. Second Stage Algorithm in place
30. Established policy and criteria for operative vaginal
delivery ( forceps and vacuums).
31. Any dual mode delivery reviewed (vacuum-forceps;
forceps-cesarean; etc).
32. Established neonatal hand off criteria
Structure -Birth
33. NRP personnel available at birth
34. Skin to skin is an option in all births (vaginal and
cesarean) and for all designees (mother, significant
other)
35. Breastfeeding occurs in the first hour (if applicable)
as standard
36. Identification of neonates in the Late Preterm
Segment to deploy resources to Mom and Baby.
(LPI Toolkit)
37. Family is not separated for administrative reasons,
only clinical.
Structure- Postpartum
38. Rooming in is the standard
39. Lactation support available to all mothers
40. Identification of Moms needing a Home Visit after
discharge
41. Established relationship with Care
Management(Health Plan) in facility
* (#7): Individual Provider Data Published
NICHD Workshop Recommendations for local adoption-# failed inductions, # not
meeting criteria for indication, # cesarean sections after induction
3