Lewis: Medical-Surgical Nursing, 7th Edition
advertisement
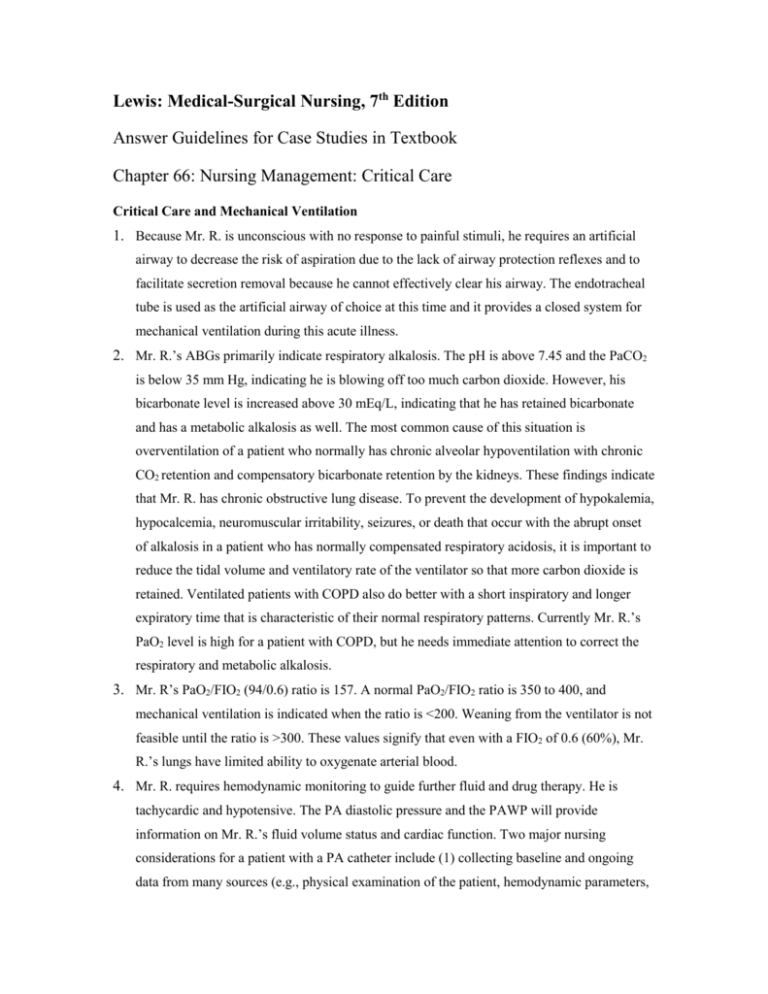
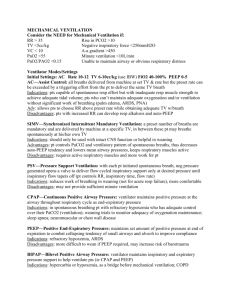
Lewis: Medical-Surgical Nursing, 7th Edition Answer Guidelines for Case Studies in Textbook Chapter 66: Nursing Management: Critical Care Critical Care and Mechanical Ventilation 1. Because Mr. R. is unconscious with no response to painful stimuli, he requires an artificial airway to decrease the risk of aspiration due to the lack of airway protection reflexes and to facilitate secretion removal because he cannot effectively clear his airway. The endotracheal tube is used as the artificial airway of choice at this time and it provides a closed system for mechanical ventilation during this acute illness. 2. Mr. R.’s ABGs primarily indicate respiratory alkalosis. The pH is above 7.45 and the PaCO2 is below 35 mm Hg, indicating he is blowing off too much carbon dioxide. However, his bicarbonate level is increased above 30 mEq/L, indicating that he has retained bicarbonate and has a metabolic alkalosis as well. The most common cause of this situation is overventilation of a patient who normally has chronic alveolar hypoventilation with chronic CO2 retention and compensatory bicarbonate retention by the kidneys. These findings indicate that Mr. R. has chronic obstructive lung disease. To prevent the development of hypokalemia, hypocalcemia, neuromuscular irritability, seizures, or death that occur with the abrupt onset of alkalosis in a patient who has normally compensated respiratory acidosis, it is important to reduce the tidal volume and ventilatory rate of the ventilator so that more carbon dioxide is retained. Ventilated patients with COPD also do better with a short inspiratory and longer expiratory time that is characteristic of their normal respiratory patterns. Currently Mr. R.’s PaO2 level is high for a patient with COPD, but he needs immediate attention to correct the respiratory and metabolic alkalosis. 3. Mr. R’s PaO2/FIO2 (94/0.6) ratio is 157. A normal PaO2/FIO2 ratio is 350 to 400, and mechanical ventilation is indicated when the ratio is <200. Weaning from the ventilator is not feasible until the ratio is >300. These values signify that even with a FIO2 of 0.6 (60%), Mr. R.’s lungs have limited ability to oxygenate arterial blood. 4. Mr. R. requires hemodynamic monitoring to guide further fluid and drug therapy. He is tachycardic and hypotensive. The PA diastolic pressure and the PAWP will provide information on Mr. R.’s fluid volume status and cardiac function. Two major nursing considerations for a patient with a PA catheter include (1) collecting baseline and ongoing data from many sources (e.g., physical examination of the patient, hemodynamic parameters, laboratory values) to evaluate the effectiveness of interventions, and (2) observing the patient for signs of complications related to the PA catheter (e.g., infection, air embolus). 5. Mr. R.’s PAWP is high, his CI is low, and his SVR is high. These values indicate heart failure, most likely from the dysrhythmia. Medical interventions would be aimed at treating the heart failure and could include initiation of drug therapy (e.g., dobutamine, digoxin), cardioversion to convert Mr. R.’s rhythm to normal sinus, and placement of an intraaortic balloon pump to provide temporary circulatory assistance should his condition worsen. 6. PPV affects circulation because of the transmission of increased mean airway pressures to the thoracic cavity. The increased intrathoracic pressure compresses thoracic vessels and consequently decreases venous return (preload) and CO. Mean airway pressure is further increased if PEEP is added to improve oxygenation. Generally, PEEP is contraindicated or used with extreme caution in patients with highly compliant lungs as occurs in the patient with COPD. Assuming that Mr. R.’s heart failure is corrected, the addition of PEEP may place him at risk for a subsequent reduction in CO/CI and/or barotrauma secondary to PEEP. 7. Nursing diagnoses: ineffective airway clearance, decreased cardiac output Collaborative problems: barotrauma, sepsis The nurse would coordinate the meeting by assuring that key family and health care team members (e.g., physicians, clergy) were in attendance. In addition, the nurse would contribute to the meeting by serving as an advocate for the patient and family members