5_Liver,Gall,Pancreas - V14-Study
advertisement
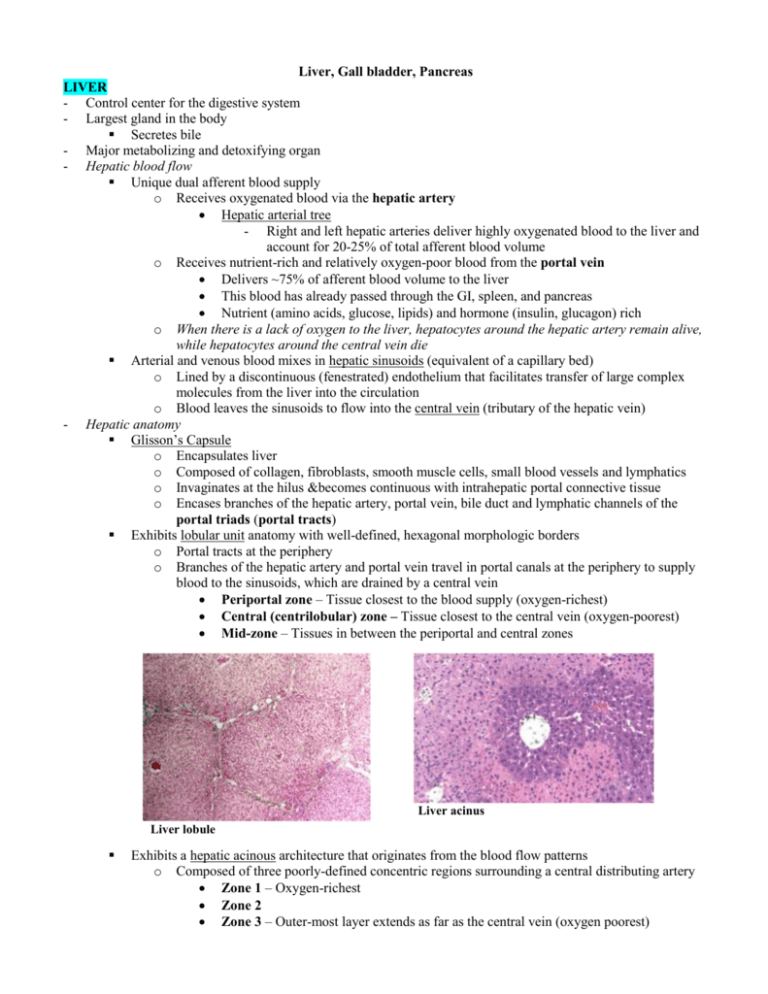
Liver, Gall bladder, Pancreas LIVER - Control center for the digestive system - Largest gland in the body Secretes bile - Major metabolizing and detoxifying organ - Hepatic blood flow Unique dual afferent blood supply o Receives oxygenated blood via the hepatic artery Hepatic arterial tree - Right and left hepatic arteries deliver highly oxygenated blood to the liver and account for 20-25% of total afferent blood volume o Receives nutrient-rich and relatively oxygen-poor blood from the portal vein Delivers ~75% of afferent blood volume to the liver This blood has already passed through the GI, spleen, and pancreas Nutrient (amino acids, glucose, lipids) and hormone (insulin, glucagon) rich o When there is a lack of oxygen to the liver, hepatocytes around the hepatic artery remain alive, while hepatocytes around the central vein die Arterial and venous blood mixes in hepatic sinusoids (equivalent of a capillary bed) o Lined by a discontinuous (fenestrated) endothelium that facilitates transfer of large complex molecules from the liver into the circulation o Blood leaves the sinusoids to flow into the central vein (tributary of the hepatic vein) - Hepatic anatomy Glisson’s Capsule o Encapsulates liver o Composed of collagen, fibroblasts, smooth muscle cells, small blood vessels and lymphatics o Invaginates at the hilus &becomes continuous with intrahepatic portal connective tissue o Encases branches of the hepatic artery, portal vein, bile duct and lymphatic channels of the portal triads (portal tracts) Exhibits lobular unit anatomy with well-defined, hexagonal morphologic borders o Portal tracts at the periphery o Branches of the hepatic artery and portal vein travel in portal canals at the periphery to supply blood to the sinusoids, which are drained by a central vein Periportal zone – Tissue closest to the blood supply (oxygen-richest) Central (centrilobular) zone – Tissue closest to the central vein (oxygen-poorest) Mid-zone – Tissues in between the periportal and central zones Liver acinus Liver lobule Exhibits a hepatic acinous architecture that originates from the blood flow patterns o Composed of three poorly-defined concentric regions surrounding a central distributing artery Zone 1 – Oxygen-richest Zone 2 Zone 3 – Outer-most layer extends as far as the central vein (oxygen poorest) - - Bile duct and canaliculi Transport bile out of the liver o Hepatocytes absorb bilirubin from blood, conjugate and secrete into bile canaliculi Canaliculi are minute spaces between hepatocytes formed by tight junctions o Bile flows from canaliculi to bile ductules (cholangioles) Ductules are lined by simple cuboidal epithelium - Epithelial cells are called cholangiocytes Ductules transition into interlobular bile ducts - Lined by simple cuboidal or columnar epithelium and Interlobular bile ducts flow into intrahepatic and hepatic duct Cells of liver parenchyma Hepatocytes o 80% of cell population o Arranged in hepatic cords or plates o Large polyhedral cells o Round, centrally-located nuclei Frequently polyploidy (>1 nucleus) o Specialized surface depending on cell orientation Microvillous surfaces face perisinusoidal space Canalicular surfaces face border bile canaliculi Sinusoidal endothelial cells Hepatic sinusoids o Line fenestrated wall of hepatic sinusoids Endothelial cell fenestrations prevent RBCs but allow plasma to pass into the Space of Disse in order to contact hepatocyte microvilli o Separated from the hepatocytes by an interstitial, perisinusoidal space (Space of Disse) Space is important because anything there has direct contact with hepatocytes Space pathology (e.g. fibrosis) will prevent normal contact of plasma with hepatocytes Sinusoidal endothelial cells Space of Disse Stellate cells Ito cells (stellate cells) o Located in the space of Disse o Involved in production of extracellular matrix components found within the Space of Disse o Secrete cytokines (inflammatory mediators) important in liver maintenance, growth, and repair o Major function when quiescent Storage of Vitamin A and other lipid-soluble vitamins Kupffer cells o Located in hepatic sinusoids o Resident liver macrophages responsible for phagocytosis Phagocytose bacteria and particulate matter Degrade bacterial endotoxin o Remove damaged RBCs and other cellular molecules Contain iron from phagocytosed RBCs Contain lipofuscin and ceroid from lipid metabolism Secrete cytokines Functions as antigen-presenting cells Involved in tumor cell surveillance o o o Kupffer cells GALL BALDDER - Concentrates bile via coupled active transport of salt and water Epithelial cells transport Na+, Cl-, and HC03- ions from cytoplasm into intercellular space, which creates an osmotic gradient that encourages water to move into the intracellular space - Microanatomy Tunica mucosa o Very regular simple columnar epithelium o No goblet cells or glands Deep folds of the mucosa sometimes look like "glands," but they really are parts of the lumen that disappear on distention and have no secretory activity Propria submucosal Lamina propria (small) Tunica muscularis (thin and stringy) Tunica adventitia (dense CT) o Continuous with Glisson’s capsule of the liver No muscularis mucosae or submucosa PANCREAS - Has both exocrine and endocrine functions Pancreas is mostly composed of exocrine tissue o Synthesize the bulk of the digestive enzymes needed by the intestines, that travel via a duct system to the duodenum o Impairment of this function leads to maldigestion, malabsorption, and eventual death Consequently, pancreatic inflammation and cancer are quite lethal Endocrine tissue o Consists of Islets of Langerhans scattered throughout exocrine tissue Pancreas o Endocrine products enter blood directly - Anatomy of Exocrine Pancreas Acinar tissue o Basic secretory unit is the acinus cell Acinar cells arranged into blind-ended acini (like in other glands) Cells have a deeply basophilic basal region - Due to presence of large amounts of rER Cells have an eosinophilic apical region - Contains distinct zymogen granules Precursor forms of digestive enzymes Granule membranes fuse with the plasma membrane and contents are released into ducts via exocytosis o Secretory cells are grouped around a small lumen into which secretions are released Secretory product is stored in vesicles (derived from the Golgi apparatus) and held in the apical cytoplasm until a signal is received to release them Once the signal is received, inactive secretory products are released into ducts Secretory products become activated when they reach the intestine - The release of active forms into ducts would destroy pancreatic tissue Ducts o Duct system begins in the acinus (unique feature) o First part of the duct system is lined by small centroacinar cells o Centroacinar cells form intercalated ducts Lined by low columnar or cuboidal epithelium o Intercalated ducts empty into interlobular ducts Lined by a columnar epithelium o Interlobular ducts empty into the main pancreatic duct Lined by a tall columnar epithelium Endocrine pancreas o Islets of Langerhans Regions of lighter-staining tissue scattered throughout exocrine tissue Demarcated by very fine CT fibrils Well vascularized (as you would expect in any endocrine organ) Contain various cell types - Mostly (beta) β-cells – secrete insulin - (Alpha) α-cells – secrete glucagon - (Delta) δ-cells – secrete somatostatin - Other islet cells secrete hormones that include pancreatic polypeptide, vasoactive intestinal peptide, secretin, and motilin All of the individual islet cells islets look the same Endocrine pancreas Exocrine pancreas