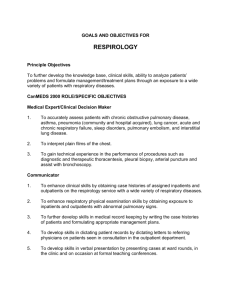
Post Operative Pulmonary Complications
advertisement

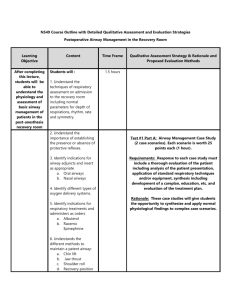
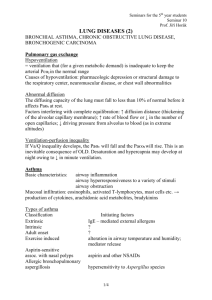
- Postoperative Pulmonary Complications – Can Preoperative Evaluation Help to Identify Who Will Fail in the PACU? Defined as atelectasis, PNA, respiratory failure, exacerbation of existing lung disease, bronchospasm. PE, pulmonary edema, TROLI are separate entities in some literature, but included in others. 60-70% of major PACU complications linked to respiratory related causes, most frequently airway obstruction, hypoxemia, hypercapnia and aspiration. Study by Rose, et al., of >24000 pts, demonstrated risk of respiratory event at 1.3% combined (hypoxemia 0.9%, hypoventilation and obstruction at 0.2%. o Risk factors IDed: age >60 diabetic, males, obese, emergent surgery or procedures > 4 hrs (3 in other literature), use of opiates and premedication, and thiopental (vs propofol) o Those studied with an event had higher rates of additional cardiac events and ICU admissions. o Surgery related risk factors – remember close to diaphragm, greater the risk. (AAA repairs, thoracic and abdominal sx all high). Think damage to diaphragm and splinting which lowers FRC and VC Additional study with 3970pts with no cardiac surgery, the risk was highest for pulmonary complications (vs. MI, PNA) GA higher than regional/neuraxial (reductionin PNA, respiratory depression and overall mortality lowest if GA avoided) Pulmonary Pre-Op Evaluation – whats the stance? Pt with preexisting lung disease should be evaluated by clinical history for changes in severity. Smoking history is very important Some evidence based guidelines for periop pulmonary evaluation and risk staratification for noncardiothoracic surgery o Some agreement with previous risks: advanced age, ASA ≥2, noncompensated CHF, poor functional capacity, and COPD all with increased risk. o Smoking showed modest increase, while asthma and obesity did not (OSA without enough evidence to prove). Radiographs? Although commonly ordered, and abnormal CXRs have correlated with ince risk of pulmonary complications, general consensus is most information gleamed from clinical history/exam. o Meta analysis of 21 studies with >14000 pts showed abn CXR in 10% of tests, but only 1.3% were unexpected based on exam, and only 0.1% had affect on management. o ACP recommends CXR for pts over 50 with known CPD, with high risk procedures (listed above). PFTs – rarely indicated before sx, and not showen to predict periop risk better than clinical assessment, and no established cutoff values for spirometry to guide decisions. o Consider preop PFTs for new, unexplained symptoms, or unclear clinical picture. If vitals capacities are <35% predicted are associated with increase in risk for mechanical ventilation. o Always done for lung reduction surgery o Consider aggressive periop optimization of symptoms, with bronchodilators, or short course of systemic steroids. Larger reduction in postop pulm complications by conventional lung expansion treatments (deep breathing, ICS, BIPAP (as good as ICP), and CPAP. Previous studies with 50% reduction in postop complications Epidural post op pain control and NG decompression after abdominal sx Other disease (neuromuscular, orthopedic such as scoliosis, CHD, RV failure, and anticipated blood loss > 30 ml/kg Mechanism of Dysfunction Inadequate postop ventilation expect mild respi academia with slightly elevated PaCO2s o watch if coincident with tachypnea, dyspnea, laboredbreathing, anxiety (all appear to be “not enough pain relief”) o <7.30 or progressive inc in PaCO2 is conserning. Decreased Respiratory Drive – likely 2/2 residuat IV or inhalational agents, all blunt both hypoxic and hypercapneic responses. o Pt with recent opiate tx, can report good relief, but gradually become hypoventilatory – need to balance pain control with necessary ventilator response (narcan and flumazenil) o Other to consider, ICH/edema or chronic respiratory acidosis from COPD (hypoventilation from supplemental O2 rarely occurs) o All patients should receive oxygen therapy by facemask (at 40%) or nasal prongs (4L/min). Healthy patients may not require oxygen therapy after a brief minor surgical procedure, guide with SaO2. Increased Airway Resistance – generally causes by physical obstruction or edematous tissues, incomplete NMB reveral, or unknown neuromuscular disorders. o Chin lift with OP airway first line, NP is better tolerated. o Laryngospasm treated with chin lift, consider PP ventilations and then succinlycholine, if airway edema appears to worsen, consider nebulized vasoconstircots. o Treatment of small airway dz with nebulized albuterol/ inhaled steroid. Inadequate PostOp Oxygenation – overall changed in metabolic status can alter this; sepsis, hypotension and anemia can also do this If closing capacity exceeds FRC, airways collapse during tidal breathing and an intrapulmonary shunt develops thus increasing risk of hypoxemia. With reduced closing capacity (with inc age) or reduced FRC y (pulmonary edema, infection, aspiration, obesity) Decreased Lung Compliance – reduction in FRC leads to small airway closure, watch for tight dressings Increased Dead Space – high dead space ratio shows inc risk of pulm complication. PE, thrombus or debris can cause this VQ mismatching – from atelectasis , dependant portions of lung perfused but nonventilated, lung zone switching when supine. References: Rose DK, Cohen MM, Wigglesworth DF: Critical respiratory events in the postanesthesia care unit. Patient, surgical and anesthetic factors., Anesthesiology 1994; 81:410 Noninvasive ventilation.Barreiro TJ - Crit Care Clin - 01-APR-2007; 23(2): 201-22, ix Critical care challenges in orthopedic surgery patients.Taylor JM - Crit Care Med - 01-SEP-2006; 34(9 Suppl): S191-9 Pleural effusions of extravascular origin.Sahn SA - Clin Chest Med - 01-JUN-2006; 27(2): 285-308 Miller: Miller's Anesthesia, 6th ed., 2005 RESPIRATORY FUNCTION DURING ANESTHESIA Perioperative medicine for the hospitalized patient.Grant PJ - Med Clin North Am - 01-MAR-2008; 92(2): 325-48, viii