bronchiectasis, lung absces, cystic fibrosis, pulmonary fibrosis
advertisement

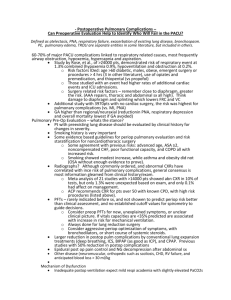
Seminars for the 5th year students Seminar 10 Prof. Jiří Horák LUNG DISEASES (2) BRONCHIAL ASTHMA, CHRONIC OBSTRUCTIVE LUNG DISEASE, BRONCHOGENIC CARCINOMA Pulmonary gas exchange Hypoventilation = ventilation that (for a given metabolic demand) is inadequate to keep the arterial PCO2 in the normal range Causes of hypoventilation: pharmacologic depression or structural damage to the respiratory center, neuromuscular disease, or chest wall abnormalities Abnormal diffusion The diffusing capacity of the lung must fall to less than 10% of normal before it affects PaO2 at rest. Factors interfering with complete equilibration: ↑ diffusion distance (thickening of the alveolar capillary membrane); ↑ rate of blood flow or ↓ in the number of open capillaries; ↓ driving pressure from alveolus to blood (as in extreme altitudes) Ventilation-perfusion inequality If Va/Q inequality develops, the PaO2 will fall and the PaCO2 will rise. This is an inevitable consequence of OLD. Desaturation and hypercapnia may develop at night owing to ↓ in minute ventilation. Asthma Basic characteristics: airway inflammation airway hyperresponsiveness to a variety of stimuli airway obstruction Mucosal infiltration: eosinophils, activated T-lymphocytes, mast cells etc. → production of cytokines, arachidonic acid metabolites, bradykinins Types of asthma Classification Extrinsic Intrinsic Adult onset Exercise induced Aspirin-sensitive assoc. with nasal polyps Allergic bronchopulmonary aspergillosis Initiating factors IgE – mediated external allergens ? ? alteration in airway temperature and humidity; mediator release aspirin and other NSAIDs hypersensitivity to Aspergillus species 1/4 Seminars for the 5th year students Seminar 10 Prof. Jiří Horák Dg: episodic dyspnea with wheezing, intermittent cough; symptoms are worse at night Lab.: decreased FEV1 (improvement with bronchodilator); portable peak-flow measurements; skin tests – demonstrate atopy; blood tests – eosinophilia and IgE increase Status asthmaticus – an attack of increased severity that is unresponsive to routine therapy. The degree of severity is best appreciated by a measure of expiratory flow rates. Hypoxemia is usually present. PaCO2 is typically ↓ early in an attack. With increasing severity, PaO2 falls and PaCO2 returns to normal and then rises. Chronic obstructive pulmonary disease (COPD) = slowly progressive airway obstruction with periodic exacerbations (↑ in dyspnea and sputum production). Clin: dyspnea, exercise intolerance, cough, sputum production. Phys: lung overinflation, prominent use of accessory respiratory muscles, diminished breath sounds, expiratory wheezing; pink puffer, blue bloater. Dg: in early stages the physical examination may be normal → diagnosis depends on ↓ expiratory flow rates. Spirometry: ↓ VC and expiratory flow rates, ↑ RV, FRC and TLC. Bronchodilators can often ↑ expiratory flow. Arterial blood gases: hypoxemia of varying severity; hypercapnia is seen in advenced stages only. Severe hypoxemia → anatomic remodeling of pulmonary arteries → pulmonary hypertension and subsequent right heart failure (cor pulmonale). Secondary polyglobulia. Emphysema Def: abnormal enlargement of the air spaces distal to the terminal bronchioles due to destructive changes in the alveolar walls. The degree of airway obstruction in patients with COPD correlates closely with the severity of emphysema. Pathol: imbalance of proteases and antiproteases in the lung → lung destruction Dg: physical examination, X-ray, ↓ diffusing lung capacity Small airway disease Inflammation of the terminal and respiratory bronchioles, fibrosis of the airway leading to narrowing, goblet cell metaplasia → airway obstruction 2/4 Seminars for the 5th year students Seminar 10 Prof. Jiří Horák Chronic bronchitis Def: persistent cough with sputum production for › 3 months in each year over three years Th: symptomatic, reduction of the abnormal airway tone, treatment of inflammation and specific complications (infection, excessive bronchial secretions, hypoxemia, cor pulmonale) Smoking cessation Pharmacologic therapy Sympathomimetics - beta2-specific agents: metaproterenol, terbutaline, albuterol - epinephrine Methylxanthines - theophylline - aminophylline Anticholinergics - atropine - ipratropium bromide Anti-inflammatory drugs - corticosteroids - cromolyn sodium Oxygen Antibiotics Lung cancer - the leading cause of death causative factors: cigarette smoking – responsible for up to 90% of cases 4% of those who have smoked for 40 years develop cancer 2% of new lung cancer cases are due to passive smoking exposure all types except bronchoalveolar carcinoma are associated with smoking asbestos (esp. + smoking) – 14% of smokers with asbestosis develop lung cancer - small-cell and non-small cell carcinoma secondary tumours: - metastatic spread of neoplasma to the lung: lung parenchyma, bronchial mucosa, chest wall, pleural space, mediastinum - direct extension (the least common): breast, liver, pancreas - hematogenous: renal, thyroid, testicular tumours, bone sarcomas 3/4 Seminars for the 5th year students Seminar 10 Prof. Jiří Horák Clin: cough, weight loss, hemoptysis, dyspnea, chest pain Pancoast‘s syndrome Horner‘s syndrome superior vena cave syndrome postobstructive pneumonia hoarseness (paresis of left n. recurrens) pleural or pericardial effusion paraneoplastic syndromes in 10 – 50% of patients: - hypertrophic pulmonary osteoarthropathy - gynecomastia - syndrome of inappropriate ADH secretion - hypercalcemia - Cushing‘s syndrome - Eaton-Lambert myasthenic syndrome - thrombophlebitis metastases: brain, liver, bone, lymph nodes Dg: laboratory tests, X-ray, CT scan, bronchoscopy, biopsy Th: surgery – for non-small cell carcinoma radiation therapy – not beneficial in non-small cell carcinoma chemotherapy in small cell carcinoma limited to the thorax prolongs survival from 3 to 16 months The 5-year survival rate for all patients with bronchogenic carcinoma is about 10% -------------------- 4/4