Respiratory Failure and ARDS
advertisement

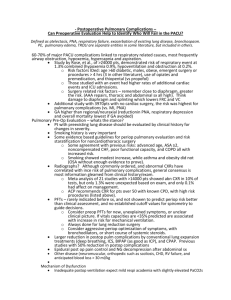
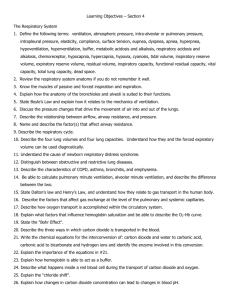
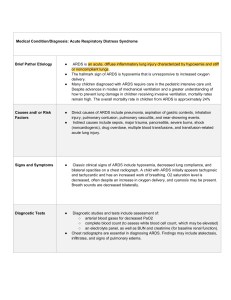
UTHSCSA Pediatric Resident Curriculum for the PICU RESPIRATORY FAILURE & ARDS RESPIRATORY FAILURE Inability of the pulmonary system to meet the metabolic demands of the body through adequate gas exchange. Two types of respiratory failure: Hypoxemic Hypercarbic Each can be further divided into acute and chronic. Both types of respiratory failure can be present in the same patient. CENTRAL ETIOLOGIES Trauma: head injury, asphyxiation, hemorrhage Infection: meningitis, encephalitis Tumors Drugs: narcotics, sedatives Neonatal apnea Severe hypoxemia or hypercarbia Increased ICP from any of the above causes OBSTRUCTIVE ETIOLOGIES Upper Airway Lower Airway Anatomic: choanal atresia, tracheomalacia, tonsillar hypertrophy, laryngeal web, vascular rings, vocal cord paralysis, macroglossia Aspiration: mucus, foreign body, vomitus Infection: epiglottitis, abscesses, laryngotracheitis Tumors: hemangioma, cystic hygroma, papilloma, Laryngpospasm Anatomic: bronchomalacia, lobar emphysema Aspiration: FB, mucus, meconium, vomitus Infection: pneumonia, pertussis, bronchiolitis, CF Tumors: teratoma, bronchogenic cyst Bronchospasm RESTRICTIVE ETIOLOGIES Lung Parenchyma Chest Wall Anatomic: agenesis, cyst, pulmonary sequestration Atelectasis Hyaline membrane disease ARDS Infection: pneumonia, bronchiectasis, pleural effusion, Pneumocystis carinii Air leak: pneumothorax Misc: hemorrhage, edema, pneumonitis, fibrosis Muscular: diaphragmatic hernia, myasthenia gravis, muscular dystrophy, botulism Skeletal: hemivertebrae, absent ribs, fused ribs, scoliosis Misc: distended abdomen, flail chest, obesity HYPOXEMIA V/Q mismatch Most common reason. Blood perfuses non-ventilated lung. Seen in atelectasis, pneumonia, bronchiectasis Global hypoventilation: apnea Right-to-left shunt Intracardiac lesions, e.g., tetralogy of Fallot Incomplete diffusion Oxygen must diffuse across increased distance secondary to interstitial edema, fibrosis, or hyaline membrane. Low inspired FiO2: high altitude HYPERCARBIA Pump Failure Reduced central drive: apnea, metabolic alkalosis, drugs, brainstem injury, hypoxia Muscle fatigue: muscular dystrophy Increased pulmonary workload: decreased compliance, increased obstruction Increased CO2 production: fever, seizure, malignant hyperthermia Increased dead space: V/Q mismatch (ventilation of non-perfused lung) PHYSICAL EXAM Tachypnea Dyspnea Retractions Nasal flaring Grunting Diaphoresis Tachycardia Hypertension Altered mental status Confusion Agitation Restlessness Somnolence Cyanosis (need 5mg/dl of unoxygenated blood) CXR FINDINGS CXR may be normal if problem is with upper airway Can see hyperinflation, atelectasis, infiltrate, cardiomegaly Additional studies may be needed, e.g., chest CT, barium swallow, echocardiogram BLOOD GAS For any age patient, breathing room air, respiratory failure is defined as arterial pCO2 > 50mm Hg or arterial pO2 < 60mm Hg. If the patient is hyperventilating, a normal pCO2 is disturbing. The above definition assumes the absence of an anatomic shunt. Chronic hypercarbic respiratory failure will often have a normal pH because of compensatory metabolic alkalosis. MANAGEMENT REMEMBER PALS Airway Breathing Circulation AIRWAY Repositioning Position of comfort Jaw thrust/chin lift Oral airway Unconscious patients only Nasal trumpet Nasal or mask CPAP Bag-mask ventilation Use during preparation for intubation Tracheal intubation BREATHING Decrease respiratory workload ß-agonists Decadron or steroids Antibiotics CPAP Supplemental O2 Nasal cannula Closed face mask Non-rebreather Counteract drug effects Bag-mask ventilation Mechanical ventilation CIRCULATION Suppress anaerobic metabolism and acidosis Correct anemia to improve oxygen delivery Ensure adequate cardiac output Inotropes: oxygen, vasopressors Fluid boluses ARDS A patient must meet all of the following: Acute onset of respiratory symptoms CXR with bilateral infiltrates No evidence of left heart failure PaO2/FiO2 < 200mm Hg (regardless of PEEP) American-European Consensus Conference on ARDS (Am J Resp Crit Care Med 149:818, 1994) The following are implied: Previously normal lungs Decreased lung compliance Increased shunting Hypoxemic respiratory failure ETIOLOGY ARDS represents about 3% of PICU admissions. Numerous precipitating events: Trauma Pneumonia Burns Sepsis Drowning Shock PATHOPHYSIOLOGY Acute Injury Latent Period Early Exudative Phase Cellular Proliferative Phase Fibrotic Proliferative Phase Royall and Levin J Peds 112:169-180; 335-347, 1988 PATHOLOGY OF ARDS Green arrows point to hyaline membrane Blue arrows point to type II pneumocytes and alveolar macrophages MANAGEMENT Meticulous supportive care is the mainstay of therapy Prevent secondary lung injury Ensure adequate cardiac output Limit secondary infections Drugs Good nutrition VENTILATOR STRATEGIES The hallmark of ARDS is heterogeneous lung. Limit Barotrauma Keep PIP <35 cm H2O Use pressure-control ventilation Use TV of 6-10cc/kg Keep rate <30 bpm Permissive hypercapnia Use bicarb or THAM to keep pH >7.20 Limit O2 Toxicity Give enough PEEP to lower FiO2 to <60% while maintaining O2 >90%. PEEP <15 cm H2O shouldn’t decrease cardiac output. Increase mean airway pressure with inverse ratio (I>E) ventilation. CARDIAC OUTPUT Keep cardiac output >4.5 L/min/m2. Keep O2 delivery >600 ml O2/min/m2. Keep Hct >30%, higher if signs of heart failure. Use inotropes to augment cardiac output. Ensure adequate preload. LIMIT SECONDARY INFECTIONS Wash your hands. Use the gut as soon as possible for nutrition and meds. Discontinue indwelling catheters as soon as possible. Have high index of suspicion. Treat infections early, but tailor antibiotics to culture results. DRUGS Diuretics: a dry lung is a good lung. Inotropes Steroids: 2mg/kg/day begun after a week into the course may be of benefit, otherwise don’t use. Pulmonary vasodilators (nitric oxide, prostaglandins, nitroprusside): of little benefit. NO may be of benefit in some patients. Surfactant replacement: probably no benefit NSAIDs: no clinical benefit NUTRITION Ensure adequate calories as soon as possible: 50-60kcal/kg/day in infants 35-45kcal/kg/day in older children. After day 4, increase calories by 25-50% above baseline. Begin enteral feeds as soon as is safe. “Pulmonary” formulas probably of little benefit. MORTALITY/MORBIDITY Published mortality is 50% in children. Pulmonary failure accounts for only 15% of the deaths. Lung function usually returns to normal within 18 months after leaving the hospital.