cardio article - Airway clearance
advertisement
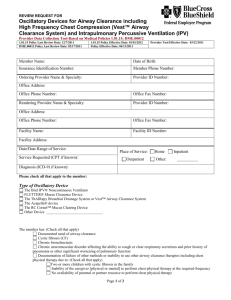
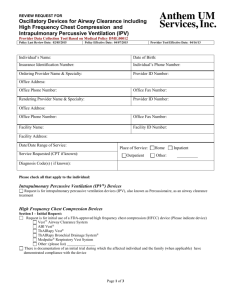
Airway clearance devices in cystic fibrosis John H. Marks Management of the pulmonary complications of cystic fibrosis (CF) patients involves airway clearance therapies (ACTs) to remove obstructing secretions from the airways. Conventional Chest physiotherapy (CCPT) is considered the ‘gold standard’ method of airway clearance for CF patients but time and need of assistance often leads to lack of adherence. Aerosolized bronchodilators and mucolytics have been used to aid airway clearance by dilation of respiratory passages and breakdown secretions. Several airway clearance devices have been shown to be effective in aiding airway clearance in CF patients. Positive Expiratory Pressure (PEP) – is the simplest and least expensive device. Upon exhalation, PEP creates a resistor to generate positive pressure in the airways. Different resistance orifices allow for different pressures of 10-20cm h2o with an inspiration to expiration ratio of 1:3 or 1:4. PEP exhalation (approx 10) should be followed by a series of huffs and should be repeated several times until clear or over a 20 min interval. Flutter – provides PEP therapy with oral airway oscillations. During exhalation, pressure from the airways is transmitted to the flutter causing the steel ball to bounce creating several opening and closing cycles with each breath. PEP develops in the range of 10-25 cm h2o at an oscillatory frequency of about 15 Hz, lifting the device adjusts the frequency to achieve the greatest amount of airway vibration. Several series of 5-10 exhalations followed by 1 or 2 forceful exhalations and huff coughs over 10-20mins. Acapella – same principle as flutter, but not gravity dependant. Three models: low flow(less than 15L/min), high flow (greater than 15L/min) and the acapella choice – can be used in line with a nebulizer. RC cornet – consists of a semi circular tube containing a flexible latex free hose. Expiration through the hose causes it to flex, buckle and unbuckle causing oscillatory positive pressure in the airways which fluctuates many times per second. Intrapulmonary Percussive Ventilation (IPV) – delivers small bursts of air through a mouthpiece at a rate 200-300 cycles per min (2-5 Hz) using a sliding venture to cause rapid flow interruptions. It entrains an aerosol of up to 20ml of saline with or without a bronchodilator over about 20 mins. Optimal effect achieved by pressure and frequency is determined by direct observation of chest movement and patient comfort. Oscillations occur mainly during inhalation. The presumed mechanism of action of the IPV include bronchodilationfrom increased airway pressure and delivery of nebulized bronchodilator, prevention of airway collapse, improved distribution of ventilation and stimulation of cough. Percussive Nebulizer – is an oral intrapulmonary percussive treatment device that incorporates a large volume nebulizer (20ml) for delivery of aerosolized medication with oscillating positive pressure. Oscillatory frequency ranges from 6 to 30 with airway pressures of 6–15 cm H2O. The PNeb oscillates during both inhalation and exhalation, enhancing aerosol delivery and maintaining airway patency. Presumed mechanisms of action are similar to the IPV and include bronchodilation, prevention of airway collapse and shearing of mucus from airway walls, and possible thinning of secretions by high expiratory percussive flow. High frequency chest wall oscillation - There are two devices utilizing an inflatable vest connected to an air-pulse generating compressor to deliver high-frequency chest wall oscillation (HFCWO), The Vest and the SmartVest.The airpulse generator rapidly inflates and deflates the vest, gently compressing and releasing the chest wall several times per second. Oscillation frequency can be adjusted from 5 to 25 Hz with pressure to the vest ranging from 3 to 25 cm H2O. The chest wall oscillations are transmitted to the airways creating mini-coughs. Treatment sessions generally last 20 to 30 min and consist of short segments at different frequencies separated by huff coughs. The proposed mechanism of action of HFCWO is enhancement of mucus transport in three essential ways: by altering the rheologic properties of mucus, by creating a cough-like expiratory airflow bias that shears mucus from the airwaywalls, and by enhancing ciliary beat frequency, all of which help move mucus toward central airways. HFCWO has also been shown to improve distribution of ventilation.One study found that patients with moderate or severe airway obstruction may benefit fromlower vest pressures at frequencies of 10–15 Hz to minimize decrease in end-expiratory lung volume and maximize oscillatory flow.