When the patient meets all extubation criteria, she should be
advertisement

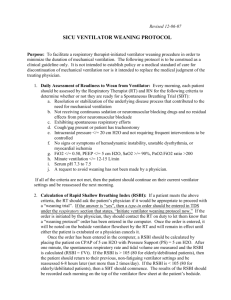
Chapter 10, Case Study, Airway Management and Ventilatory Support 1. Describe appropriate weaning goals for Mrs. Q., based on her status today. What ventilator settings should be used? Ventilatory weaning: Goal for the day: to lower inspiratory pressure limit (IPL) to 10 or even 5 cm H2O and assess the patient’s response to those changes. o The tidal volume and minute volume may drop, respiratory rate should remain less than 25 breaths/minute, and she should not use her accessory muscles. o Her SaO2 should remain well above 90% or if it falls, she should be put back to the previous IPL level of 14 cm H2O and monitored for all parameters to stabilize. The weaning trials then would pause until later in the day or the next day following Society of Critical Care Medicine guidelines to allow rest between spontaneous breathing trials and at least 12 to 24 hours rest for a weaning trial failure. Ventilator settings: The current ventilator settings are almost at minimum for a spontaneous breathing trial and possible extubation. 2. When would Mrs. Q. be considered ready for extubation? What weaning assessment and laboratory tests, including arterial blood gases and chemistry, should be obtained before a second trial extubation? Stability of all parameters, including respiratory rate and volumes Negative inspiratory pressure and positive expiratory pressure, which can evaluate respiratory muscle strength. Laboratory tests: Arterial blood gases and pH Chemistry for calcium, potassium, magnesium, and phosphorus Hematocrit Daily chest film, which should be reviewed for pulmonary edema or signs of pneumonia and atelectasis Thyroid panel, because a hypothyroid state could contribute to failure to wean. When the patient meets all extubation criteria, she should be extubated. 3. This is day 7 of ventilation following a failed extubation trial on the day of surgery, and Mrs. Q. has progressed physically. What respiratory assessments should the nurse follow while Mrs. Q. is working with physical therapy? During exercise: Monitor the patient’s heart rate, respiratory rate, and SaO2, which should remain above 90%. Ask if she is tiring and observed for use of accessory muscles with breathing. 4. The nurse observes Mrs. Q. on continuous positive airway pressure (CPAP) for 1 hour, and she remains stable without changes to her respiratory rate, tidal volume, or minute volume, and her arterial blood gases are within normal limits. Should Mrs. Q. be extubated after this 1-hour CPAP trial if she complained of feeling exhausted (in a written note)? What additional weaning assessments should be done? Possible extubation: Evaluate the total mobility plan and weaning plan to allow rest periods and monitor each activity for contributing to exhaustion or overwork from the patient’s point of view. o When the patient complains of fatigue, you would want to fully assess her weaning plan or trial to see if it went too long. When she has rested on the ventilator for an hour or longer with return to baseline parameters for volumes, respiratory rate, and SaO2, measure the negative inspiratory pressure and positive expiratory pressure to assess her strength. o Look at other activity to see if she was worked too much or did she not sleep well last night. 4. The medical team decides to wait 1 day longer to allow Mrs. Q. to continue on the ventilator with the reduced inspiratory pressure limit at 10 cm H2O. How does reducing the inspiratory pressure limit affect Mrs. Q.’s work of breathing and the strength and endurance of her respiratory muscles? Reduction in the IPL: The work of breathing increases, allowing the patient to take on more work of breathing during weaning. o As the patient increases her work of breathing, that should exercise the respiratory costal muscles and diaphragm, improving strength and endurance. Any weaning plan should monitor for increased work of breathing and not overwork the patient without providing for rest periods between trials. Reducing the IPL even further, to 5 cm H2O, may benefit some prolonged mechanically ventilated patients who have been ventilated for weeks or months.