File - Respiratory Therapy Files

Mechanical Ventilation
PROBLEMS
Although life-saving, PPV may be associated with many complications, including:
Consequences of PPV
Aspects of volutrauma
Adverse effects of intubation and tracheostomy
Optimal Ventilatory Care
Requires
Attention to minimizing adverse hemodynamic effects
Averting volutrauma
Effecting freedom from PPV as early as possible
Common Scenarios
•
New development of hypotension
•
Acute respiratory distress (fighting)
•
Repeated sounding of High pressure alarm
•
Hypoxemia
•
Blood from the endotracheal tube
•
Problem of diagnosing VAP
Barotrauma
or
Volutrauma
•
High Paw alone insufficient to cause alveolar rupture
•
Excessive alveolar volume the likely factor leading to alveolar rupture and air dissection
•
More frequent in younger age group
•
May be difficult to detect if small in CXR
• “Stretch-induced”
Acute lung injury
Patient-ventilator Synchrony
•
Flow-targeted breath requires careful adjustment
•
Constant flow of 40-60 lpm not always adequate
•
Monitor: patient response, airway pressure/flow graphics
•
Using decelerating flow pattern may be helpful
Patient-ventilator Synchrony
•
Pressure-targeted breath is better?
Rapid pressurisation of the airway with high initial gas flow
• Match Ppl change quicker than flow pattern (difficult to assess Ppl)
• Flow is continuously adjusted by the ventilator to maintain a constant airway pressure
Patient-ventilator Synchrony
•
Any problems from pressure breaths?
Max initial flow may not be optimal in all patients depending on drive
• Adjustment of the rate of rise may be beneficial (rise time, sensitivity)
•
Pressure of what?
Proximal airway vs Ppl by muscular effort
• So! brain(NAVA) or pleural triggering helpful with a variable minute ventilation!
Weaning from Mechanical
Ventilation
Definition of Weaning
The transition process from total ventilatory support to spontaneous breathing.
This period may take many forms ranging from abrupt withdrawal to gradual withdrawal from ventilatory support.
Weaning
Discontinuation of PPV is achieved in most patients without difficulty
up to 20% of patients experience difficulty
requires more gradual process so that they can progressively assume spont. respiration
the cost of care, discontinue PPV should proceed as soon as possible
Reversible reasons for prolonged mechanical ventilation
•
Inadequate respiratory drive
•
Inability of the lungs to carry out gas exchange effectively
•
Psychological dependency
•
Inspiratory fatigue
Weaning
•
Patients who fail attempts at weaning constitute a unique problem in critical care
•
It is necessary to understand the mechanisms of ventilatory failure in order to address weaning in this population
Why patients are unable to sustain spontaneous breathing
•
Concept of Load exceeding
Capacity to breathe
•
Load on respiratory system
•
Capacity of respiratory system
Balance Load vs Capacity
• Most patients fail the transition from ventilator support to sustain spont. breathing because of failure of the respiratory muscle pump
• They typically have a resp muscle load the exceeds the resp neuromuscular capacity
Load on Respiratory System
• Need for increase ventilation increased carbon dioxide production increased dead space ventilation increased respiratory drive
• Increased work of breathing
Causes of Inspiratory respiratory muscle fatigue
• Nutrition and metabolic deficiencies: K,
Mg, Ca, Phosphate and thyroid hormone
• Corticosteroids
• Chronic renal failure
• Systemic disceases; protein synthesis, degradation, glycogen stores
• Hypoxemia and hypercapnia
• Excessive sedation
Capacity of respiratory system
• Central drive to breathe
• Transmission of CNS signal via Phrenic nerve
• Impairment of resp muscles to generate effective pressure gradients
• Impairment of normal muscle force generation
Evidence based medicine
• When to start weaning process?
• Decision making, any guideline?
How long it will take?
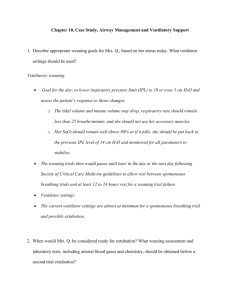
When to begin the weaning process?
• Numerous trials performed to develop criteria for success weaning, however, not useful to predict when to begin the weaning
• Physicians must rely on clinical judgement
• Consider when the reason for IPPV is stabilised and the patient is improving and haemodynamically stable
• Daily screening may reduce the duration of MV and ICU cost
Evidence-based medicine
Recommendation:
Search for all the causes that may contribute to ventilator dependence in all patients with longer than 24 h of MV support, particularly who has fail attempts. Reversing all possible causes should be an integral part of discontinuation process.
Daily Screening
• Resolution/improvement of patient’s underlying problem
• OFF potent sedation
• Adequate gas exchange (SaO
2
> 90%,
PaO
2
/FiO
2
>200)
• Respiratory rate < 35/ min
• Absence of fever, temperature < 38C
• Adequate haemoglobin concentration, > 8-10 g/dl
• Stable cardiovascular function: heart rate <
140/min, 180>SBP>90
Daily Screening (cont.)
• Indices suggesting an adequate capacity of the ventilatory pump: respiratory rate of less than 30/ min ,
• Maximum inspiratory pressure < -20 to -
30 cmH
2
O
• Correction of metabolic and electrolyte disorders
• Normal state of consciousness
Evidence-based medicine
Recommendation 2. Patients receiving
MV for respiratory failure should undergo a formal assessment of discontinuation potential if the criteria are satisfied.
Reversal of cause, adequate oxygenation, haemodynamic stability, capability to initiate respiratory effort. The decision must be individualized.
Predictions of the outcome of weaning
Variables used to predict weaning success: Gas exchange
• PaO
2 of > 60 mmHg with FiO
2 of < 0.35
•
• A-a PaO
2 gradient of < 350 mmHg
PaO
2
/FiO
2 ratio of > 200
Weaning success prediction
Ventilation Pump
• Vital capacity > 10- 15 ml/kg BW
• Maximal negative insp pressure
< -30 cmH
2
O
• Minute ventilation < 10 l/min
• Maximal voluntary ventilation more than twice resting MV
Weaning success prediction
• Tidal volume > 325 ml
• Tidal volume/BW > 4 ml/kg
• Dynamic Compliance > 22 ml/cmH
2
O
• Static compliance > 33 ml/cmH
2
O
• Rapid shallow breathing index < 105 breaths/min/L
Clinical observation of the Respiratory Muscles
• Initially thought to be reliable in predicting subsequent weaning failure
• from inductive plethysmographic studies not necessary
• a substantial increase in load will effect on the rate, depth, and pattern of breathing
• a manifestation of fatigue
Both respiratory rate and minute ventilation initially increase, may be followed by a paradoxical inward motion of the anterior abdominal wall during inspiration which indicates the insufficient diaphragmatic contraction to descend and move the abdominal content downward
Cyclic change in breathing patterns with either a chest wall motion or a predominantly abdominal wall motion are another indicator, called respiratory alternans
Fatigue Criteria
Duration of weaning prior to initial episode of fatigue (days)
Fatigue criteria
Hypoxia (PaO
2
<60, SpO2 <90%
)
Hypercarbia (PaCO
2
> 50 mmHg)
Pulse rate > 120/min
SBP > 180 or < 90 mmHg
Respiratory rate > 30/min
Clinical respiratory distress
Parameters that assess airway patency and protection
1. Maximal expiratory pressure
2. Peak expiratory flow rate
3. Cough strength
4. Secretion volume
5. Suctioning frequency
6. Cuff leak test
7. Neurological function (GCS) keep higher than 11
Evidence-based medicine
Recommendation 3.
The removal of the artificial airway from a patient who has successfully been discontinued from ventilatory support should be based on assessment of airway patency and the ability of the patient to protect the airway.
Methods of Weaning
• Abrupt Discontinuation
• Extubation to NPPV,
IPPB/IS…
• T- tube trials (ATC is preferred)
• SIMV to CPAP
• Pressure support/Volume
Support
Spontaneous breathing protocol
• Communicate with patient, weaning is about to begin, allow pt to express fear whenever possible
• Obtain baseline value and monitoring clinical parameters; vital signs, subj distress, gas exchange, arrhythmia
• Ensure a calm atmosphere, avoid sedation
• Sit the patient upright in bed or chair
• Fit T-tube with adequate flow, observe for 2 hr
For How long I will have to monitor the weaning process with SBT in my patient?
Evidence-based medicine
Recommendation 4.
Formal assessments should be done during SBT rather than receiving substantial support. The criteria to assess patient tolerance during SBTs are respiratory pattern, gas exchange, hamodynamics stability and patient comfort. The tolerance of SBTs lasting
30 to 120 minutes should prompt for permanent ventilator discontinuation.
SIMV Protocol
• Switch to SIMV from assist mode or decrease RR
• Begin with RR 8/min decrease SIMV rate by two breaths per hour unless clinical deterioration
• if assume to fail, increase SIMV rate to previous level, until stable
• if stable at least 1 hour of rate 0/ min extubate
• in patient without respiratory disorders, decrease rate with half an hour interval, 2 hr extubate
Pressure Support Protocol
•
Switch to PSV or decrease PS
•
Begin PSV at 25 cmH
2 cmH
O, decrease PS by 2-4
2
O every hour unless clinical deterioration appears , adjust pressure until stable, if stable of
PSV = 0 for at least one hour fit with T-tube or
CPAP and then observe
•
In patient without resp problems, decrease pressure at half an hour interval, if able to tolerate PSV = 0 for 2 hours, can be extubated
Failed to Wean
• Associated with intrinsic lung disease
• Associated with prolonged critical illness
• Incidence approximately 20%
• Increased risk in patient with longer duration of mechanical ventilation
• Increased risk of complications, mortality
Evidence-based medicine
Recommendation 5.
Patients receiving MV who fail an SBT should have the cause determined.
Once causes are corrected, and if the patient still meets the criteria of weaning, subsequent SBTs should be performed every 24 hours.
Evidence-based medicine
Recommendation 6.
Patients receiving MV for respiratory failure who fail an
SBT should receive a stable , nonfatiguing, comfortable form of ventilatory support.
Why a Weaning Protocol
Reduced ventilator time
Reduced weaning time; early beginning by non-physician healthcare workers
Reduced cost
Reduced complications: VAP
Evidence-based medicine
Recommendation 7.
Weaning protocols designed for nonphysician health care professionals should be developed and implemented by
ICUs. Protocols aimed at optimizing sedation should also be developed and implemented.
Evidence-based medicine
Recommendation 8.
Tracheostomy should be considered after period of stabilization on the ventilator when it becomes apparent that the patient will require prolonged MV. Tracheostomy should be performed when the patient appears likely to gain one or more benefits from the procedure.
Evidence-based medicine, cont.
• Required high levels of sedation to tolerate tube
• With marginal respiratory mechanics, lower resistance
• Derive psychological benefit from the ability to eat orally, communicate by articulated speech, enhanced mobility
• Assist physical therapy efforts
Evidence-based medicine
Recommendation 9.
Unless there is evidence for clearly irreversible disease , a patient requiring prolonged MV should not be considered permanently ventilator-dependent until
3 months of weaning attempts have failed.
Patient subgroups
Evidence-based medicine
Recommendation 10.
Anaesthesia/sedation strategies and ventilator management aimed at early extubation should be used in postsurgical patients.
SEMIQUANTITATIVE ASSESSMENT OF NEED FO
Spont.
R AIRWAY CARE
Gag
0 Vigorous 0 Vigorous
Sputum
0 None
1 Moderat
2 Weak
3 None
Sputum
Viscosity
0 Watery
1 Frothy
2 Thick
3 Tenaciou s
1 Moderate
2 Weak
3 None
Suctioning
Frequency per last 8 h
0 1 q 2-3 h
2 q 1-2 h
3 < q 1 h
)
1 1 pass
2 2 passes
3 > 3 passes
Sputum Character
0 Clear
1 Tan
2 Yellow
3 Green
RT role in Weaning from mechanical ventilation
Psychological preparation
Nurse-led weaning
• ICCN 2001: Limited evidence suggesting that nurse-led weaning may reduce ventilation time; however, not clear whether it was nurse-led aspect or the clinical protocol that produced the effect
• Superior to doctor-led weaning, has huge implications for intensive care practice
Nurse-led weaning
• ICCN 2002; Retrospective study in patients with MV longer than 7 days, reduced average duration of MV support
• Some delays occurred: sedation; protocol needed, epidural analgesia, tracheostomy; surgical vs percutaneous, some staff lacked confidence and knowledge: continuous education programme
Daily Screening
• Resolution/improvement of patient’s underlying problem
• Adequate gas exchange (SaO
PaO
2
/FiO
2
>200)
• Respiratory rate < 35/ min
2
> 90%,
• Absence of fever, temperature < 38C
• Adequate haemoglobin concentration, > 8-
10 g/dl
• Stable cardiovascular function: heart rate
< 140/min, 180>SBP>90
Daily Screening (cont.)
• Indices suggesting an adequate capacity of the ventilatory pump: respiratory rate of less than 30/ min, Maximum inspiratory pressure < -20 to -30 cmH
2
O
• Correction of metabolic and electrolyte disorders
• Normal state of consciousness
Oriented, Mental ease, Positive attitude
Psychological preparation
• Knowing the patient; personal resources, patient
• Oriented; understanding what will happen and negative responses
• Mental ease; absence of anxiety and fear
• supported operating being motivated and co-