Diabetic Ketoacidosis (DKA) Guideline: Definition, Treatment
advertisement

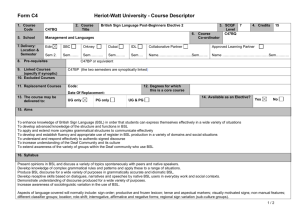
Diabetic Ketoacidosis Definition Epidemiology Pathophysiology BSL / Anion gap >10 / HCO3 <15 / pH <7.3 / moderate ketonaemia Type I > type II; 20-30% in newly diagnosed diabetes; incidence 0.5% of diabetes; most common <18yrs; Fetal mortality 30-50% Risk factors for DKA in known diabetes: poor metabolic control; low socio-economic status; previous DKA; adolescent female; psych disorder Risk Factors for DKA in unknown diabetes: <5yrs, family history of diabetes, low socio-economic status, meds (eg. High dose steroids, antipsychotics, immunosuppressants) Trigger: Concurrent infection, non-compliance with meds, MI Absolute insulin deficiency glucose uptake by cells counter-regulatory hormones – glucagon, adrenaline, growth hormon, cortisol gluconeogenesis, glycogenolysis lipolysis fatty acids overproduction of acetyl co-enzyme A ketogenesis Acetoacetate: acetoacetate:betaHB = >6:1; measured by Ketostix urine test (>3); urinary ketones may increase with treatment as beta-hydroxybutyrate is converted to acetoacetate Beta hydroxybutyrate: converted peripherally to acetoacetate; prevalent in alcoholic ketoacidosis; not detected on normal testing so ketones may be negative initially in alcoholic ketoacidosis; detected on Medisense blood test (>3) Acetone: from decarboxylation of acetoacetate excreted by kidneys and lungs; detected on Acetest (>5); responsible for ketotic breath Amino acids, Lactate glucose glycosuria, osmotic diuresis loss of H20, Na, K, Mg, PO4 hypovolaemia and lactic acidosis BSL may not be if: liver failure, alcoholic; due to impaired gluconeogenesis Investigation Check BSL hourly; continuous cardiac monitoring; accurate fluid balance; hourly neuro obs; U+E Q2-4hrly; Ca, Mg, Phos, FBC ( WBC, L shift indicated lactic acidosis), lactate; Blood culture, sputum culture: if sepsis suspected; Amylase will be factitiously increased, use lipase; Urine: ketones (positive in >95%); culture; CT head: if altered LOC VBG: raised anion gap metabolic acidosis; may get metabolic alkalosis from vomiting with anion gap as only clue of DKA; if HCO3 lower than expected for anion gap, concomitant non-anion gap metabolic acidosis (seen in patients who are still well hydrated) ETCO2: can be used in children; <29mmHg = 80% sensitivity Average body fluid deficit 5-10L (ie. 100ml/kg, 10% dehydration) Na Correct for glucose: Na + ((Glu – 5.5) / 3) Average Na deficit 5-10mmol/kg K Correct for pH: pH 0.1 = K 0.5 Average K deficit 3-5mmol/kg Osmolality Osmolality: (2 x Na) + Glu + Ur Increased Aim to BSL by no more than 5/hr, osmolality by 1-2/hr; endpoint: ketones cleared, normal anion gap Management Mild: pH >7.3, tolerating PO fluids, <5% dehydrated can consider treating with SC insulin only and not down DKA route Mod-severe: Nurse head up, NBM, NGT (if ileus), consider heparin, treat underlying cause IVF: start within 30mins of ED arrival; aim to replace total deficit over 48hrs to avoid cerebral oedema; caution in children, elderly, CCF, CRF; use N saline initially Adults Children IV FLUIDS 1L stat (if dehydrated ++) Using N saline: 1L over 1 hr 1L over 2hrs 1L over 4hrs 1L over 10hrs Add K to fluids in 2nd hour and once UO established and K <5: If K >5 = none If K 4-5 = 10mmol/hr If K 3-4 = 30mmol/hr If K <3 = 40mmol/hr 10-20ml/kg bolus N saline (if shocked, until haemodynamically stable) Calculate fluid deficit = % dehydration x weight x 10 (remember to subtract any bolus given) …and replace deficit over 48 hours If Na <150 / osmolality <320 – use N saline If Na >150 / osmolality >320 – use 0.45% saline and correct over 72hrs When BSL <15 / if BSL <10 but ongoing ketones / if BSL decreasing by >5/hr use 0.45% saline + 5% dextrose, aiming for BSL 12-15 Once K <5.5, patient PU’ing, insulin infusion started add 40mmol KCl per 1L bag Management (cntd) INSULIN Start insulin 1hr after initial fluids (only start if K >3.4, otherwise replace K first) 0.1iu/kg/hr (max 6iu/hr) actrapid insulin to 0.05iu/kg/hr when BSL <12 and acidosis improving aiming BSL 9-14; if BSL still too low despite this, can strop infusion for 10-15mins only insulin to 0.05iu/kg/hr for 4 hours if K <3 Criteria for change to SC: BSL <11, HCO3 >16-18, pH >7.3, anion gap <15, eating and drinking, normal LOC, ketones cleared; when stopping, give mixed short and long acting SC dose at least 1 hour before stopping infusion OTHERS Phosphate / Mg: only if severe / symptomatic in phosphate / Mg K2PO4 5mmol/hr MgSO4 2.5g over 1hr HCO3: only if pH <7, HCO3 <5, life-threatening hyperkalaemia, coma, haemodynamic compromise unresponsive to fluid resus May cause rapid K, worsened intracellular acidosis, impaired offloading of O 2, Na overload, hypertonicity, cerebral oedema (4x risk), volume overload, paradoxical CNS acidosis HCO3 mmol = 0.15 x base deficit x kg or 0.5-2mmol/kg over 1-2hrs Endpoint: pH >7.1, HCO3 >10 Admit ICU if: In children: <2yrs, pH <7.1, altered LOC, need for arterial line, severe hyperosmolar dehydration Discharge Patient education ( insulin by 4iu or more when intercurrent illness, even if not eating) Prognosis Mortality 5-15% (0.3-1% in children) - due to underlying disease, cerebral oedema, thromboembolism Poor prognostic factors: ARF, altered LOC, hypotension Complications Cerebral Oedema BSL, K, phosphate, ARDS, recurrence, thrombosis Leading cause of mortality from DKA; 70% mortality; 10% survivors have permanent neuro sequelae; more common in children (1% incidence) Risk factors: 1st presentation; long history poor control; <5yrs; initial corrected Na >160; severe osmolality; persistent hypoNa; severe acidosis; ??related to overaggressive fluid resus Symptoms: onset 4-12hrs after starting treatment; headache, Na, altered LOC, HR, HTN, RR, incontinence, pupil changes, seizures, papilloedema Treatment: 0.5-1g/kg mannitol IV bolus / 5-10ml/kg 3% saline IV over 30mins; give half maintenance fluids; admit PICU; neurosurg review; CT; hyperventilate if ETT Differential Diagnosis: cerebral venous sinus thrombosis (may require contrast CT / MRI for detection if initial CT normal) Differential Diagnosis Ethylene glycol, isopropyl alcohol, salicylates Other Crises New onset hyperglycaemia but no DKA: give 0.1iu/kg SC regular insulin; admit Hyperglycaemia, known diabetes, no DKA: give additional 10% of normal daily insulin dose as regular insulin SC