Endocrine Emergencies - Improving care in ED
advertisement
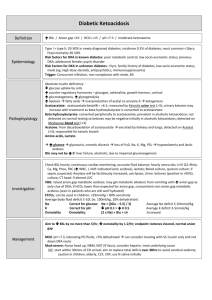
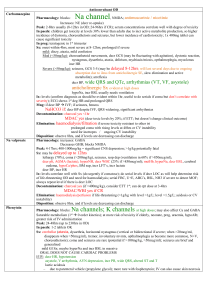
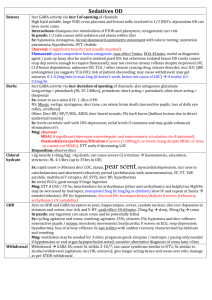
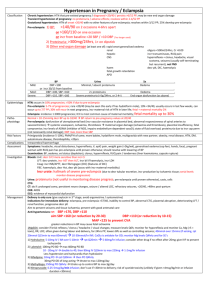
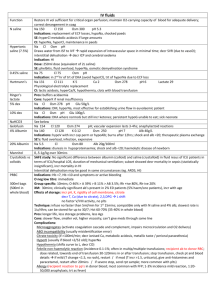
Endocrine Emergencies Name a Few… DKA HONK (HHOS) Addisonian crisis Thyroid storm Myxoedemic coma What’s the Diagnosis? 83yr woman with 3/7 histroy of malaise and polyuria. PMH type I DM and HTN HR 100, BP 100/60, GCS 14, SaO2 100% on high flow O2 Na 125 K 6.0 Cl 81 HCO3 7 Ur 25 Cr 262 Glu 54.5 Osmolality 337 DKA Definition – BSL – Ketones – Anion gap – HCO3 – pH Mortality increased present >10 <15 <7.3 5-15% (less in children) Beware if pregnant: 30-50% mortality All About Ketones Beta-hydroxybutyrate – Detected by Medisense blood test – Higher in alcoholic ketoacidosis than in DKA Acetoacetate – >6x the levels of above AFTER conversion (ie. May initially be negative) – measured by Ketostix urine test Acetone – Detected on Acetest – Responsible for ketotic breath How do ketones impact on management? – Endpoint = ketones cleared, normal anion gap Other Vital Stuff – VBG Anion gap metabolic acidosis – BSL How does BSL impact on management? Maybe metabolic alkalosis (vomiting), resp alkalosis (hyperventilation) Aim decr no more than 5/hr – Na… How do I calculate corrected Na???? Na + ( (Glu – 5.5) / 3 ) How do I correct K for pH???? Decr pH by 0.1 = Incr K by 0.5 How do I calculate osmolality? Do I even have to? Can’t I just measure it?? (2 x Na) + Glucose + Urea How does osmolality impact on management? – Aim decr by no more than 1-2/hr Any other investigations? – Average deficit 3-5mmol/kg So if pH is 7 and K is 5.7 – what is real K? How does K impact on management? – Osmolality… So if Na is 128 and Glu is 65 – what is real Na? How does Na impact on management? – K… Average deficit 5-10mmol/kg ?precipitant; ?ARF; ?level of long-term control Average body H20 deficit 100ml/kg (ie. 10% dehydration) Let’s look at that gas again… Na 125 K 6.0 Cl 81 HCO3 7 Ur 25 Cr 262 Glu 54.5 Osmolality 337 Management of DKA It’s bloody confusing and hard to remember Split into… 1) 2) 3) 4) IV fluids Potassium Insulin NaHCO3 Fluids Adult 1L stat Child 10-20ml/kg bolus rpt until haemodynamically stable 1L over 1hr 1L over 2hrs 1L over 4hrs 1L over 10hrs Replace deficit over 48hrs Deficit = %dehydration x weight x 10 Use 0.45% saline if Na >150 / Osm >320 Use N saline Use 0.45% saline and correct over 72hrs if Na >150 / Osm >320 Watch: Na, osmolality, BSL Change to 0.45% saline + 5% dex when BSL <15 and also if….. BSL decreasing too fast (ie. >5/hr) BSL <10 but ketones ongoing Potassium How do you correct for pH again? Only add K in 2nd hour / once UO / K <5 Adult – K 4-5 – K 3-4 – K <3 = 10mmol/hr = 30mmol/hr = 40mmol/hr Child – Add 40mmol to 1L bag Insulin Start after 1hr of fluids if K >3.4 (otherwise replace K first) Do you give a stat dose of actrapid? Actrapid infusion – 0.1iu/kg/hr (max 6iu/hr) – Decrease to 0.05iu/kg hr if…. BSL <12 (stop for 15mins if still too low despite this) Aim for BSL decrease of no more than 5/hr K <3 NaHCO3 What are the indications? – – – – – pH <7 HCO3 <5 Life threatening hyperkalaemia Coma Haemodynamic compromise unresponsive to IV fluids What is the dose? – 0.5 – 2mmol/kg over 1-2hrs What is the endpoint? – pH >7.1 – HCO3 >10 What are the risks? – Worsened intracellular acidosis, hypokalaemia, hypernatraemia, osmolar shifts and cerebral oedema, volume overload Cerebral oedema 70% mortality; 10% have ongoing neuro deficit; more common in children Onset 4-12hrs after starting trt What are the symptoms? – Headache, decr LOC, decr HR, incr BP, pupil changes, seizure, urinary incontinence How do you treat it? – Mannitol 0.5-1g/kg – 3% saline 5-10ml/kg over 30mins – Half maintenance fluids Hyperglycaemic Hyperosmolar State DKA HHOS Mortality up to 15% Mortality up to 45% BSL + BSL ++++ pH <7.3 pH >7.3 Anion gap >12 Anion gap <12 HCO3 <15 HCO3 >15 Ketones ++++ Ketones -/+ Maybe incr osmolality Osmolality >320-350 H20 deficit 100ml/kg (10% dehydration) H20 deficit more (20-25% dehydration) Higher Na + K deficit Resus with N saline Use N saline thereafter unless Na >150 / Osm >320 Use 0.45% saline thereafter (unless low corrected Na) Change to 0.45% saline + 5% dex when BSL <15 Replace deficit over 48hrs Replace deficit over 48-72hrs Similar K replacement Actrapid 0.1iu/kg/hr (max 6iu/hr) Actrapid 0.05iu/kg/hr (max 3iu/hr) Heparin important (hypercoag state) What’s the diagnosis (bearing in mind this is an endocrine talk)? An 85 year old man is brought to your Emergency Department fitting. His family say that he has been lethargic and weak for the last two weeks. He has a PMH of polymyalgia rheumatica. These are his initial biochemistry results. Na 99 mmol/L K 5.9 mmol/L Cl 68 mmol/L BSL 2.2mmol/L HCO3 - 21 mmol/L Urea 10.1 mmol/L Cr 180 umol/L pH 7.1 Anion gap normal pCO2 31 mmHg pO2 149.5 mmHg BE 2.4 HCO3 17.6 mmol/L Addisonian Crisis Back to Part One’s!! Effects of cortisol – Incr BSL (gluconeogenesis, lipolysis, decr ketogenesis, decr insulin release) Effects of aldosterone – Incr Na (incr reabsorption) – Decr K (incr excretion in DCT) – Alkalosis (incr H excretion) So…. what changes may be seen on bloods in view of the above? – – – – – – Dehydration – fluid resistant hypotension Decr osmolality Decr BSL Decr Na, Cl Incr K Non-anion gap metabolic acidosis – If 2Y hypoadrenalism patient euvolaemic with lower K, as aldosterone is still working Recognising Addisonian Crisis Who gets it? – 1Y – 2Y Long-term steroids stopped abruptly Adrenal haemorrhage (neonates, anticoagulated folk, sepsis (name the syndrome), trauma) Addison’s disease Prior surgical removal Adrenal destruction due to other cause: infection (eg. TB, HIV, CMV), thrombosis, metastatic Ca Head trauma Meningitis In pregnancy (name the syndrome). Pituiary failure How do they present? – Hypotension, lethargy, weight loss, weakness, N+V, abdo pain, diarrhoea – Ie. Non-specifically unwell and not responding to conventional treatment plus characteristic electrolyte changes Management Investigation – Name the investigation Management – IV fluids ++++ (vasopressors may be needed) – Dextrose – Treat K if needed – Dexamethasone 10mg IV stat (give initially as doesn’t interfere with investigations) – …then hydrocortisone 250mg IV stat What’s the diagnosis? 17yr old female presents feeling anxious, unwell, tremulous, hyperventilating, looking flushed. Recent history of abdominal pain and diarrhoea. HR 130, T 38, BP 140/87, RR 24 On examination: gallop rhythm, bibasal crepitations, abdomen SNT pH 7.8 PCO2 15 mmHg PO2 192 mmHg (75-100) Thyroid Calamities Back to Part One’s again! Effect of T3+4 – – – – Incr metabolism Incr GI motility Incr glucose absorption Incr sensitivity to epinephrine and norepinephrine, increased beta-receptors Thyroid Storm Clinical diagnosis – labs don’t differentiate Mortality 10% treated, 90% untreated with death due to CV collapse Who gets it? – Undiagnosed Graves – Meds – XS thyroxine / withdrawal from antithyroid drugs / iodine or contrast – Stressor – MI, DKA, OT Recognising Thyroid Storm Diagnostic criteria – Fever >37.8 – Incr HR out of proportion to fever (ie. >120) – CNS disturbance (eg. Altered LOC, seizures) Other – AP, N+V, diarrhoea, high output CCF (wide pulse pressure, S3 gallop rhythm), HTN, dehydration, sweating Investigations – non-specific Management A+B – Give O2 as consumption increased C – IV fluids containing dextrose – Cardioversion better than drugs for arrhythmias Treat cause Definitive treatment – Esmolol 250-500mcg/kg bolus infusion (safe as short half life; titratable; blocks cardiac and peripheral effects and slows conversion of T3 to T4) – If less severe can use PO propanolol – Hydrocortisone 100mg IV (slows conversion of T3 to T4 and decreases hormone release) – Propylthiouracil / methimazole / iodide Supportive care – Ongoing fluids, monitor electrolytes and BSL, treat fever What’s the Diagnosis? (This was an actual patient I saw last week) 58yr old man with non-specific malaise PMH: hyperthyroidism treated with radioactive iodine; known to be noncompliant with treatment OE: normal observations; mild oedema around eyes; examination otherwise unremarkable Myxoedema Coma Who’s ever seen one??? Mortality 50%; same triggers as thryoid storm Symptoms – – – – – A: hoarseness, glottic oedema B: decr RR C: decr BP, CCF D: decr LOC, hypothermia without shivering, seizures E: hypoglycaemia, paralytic ileus Management – ABC, treat cause – T3 has rapid effect, T4 has smoother improvement, give hydrocortisone – Monitor electrolytes esp Na and titrate fluids accordingly – Rewarming Anything else you want to talk about…? Hyponatraemia? Hypernatraemia? Metabolic acidosis? Sodium bicarb use?