OSCE 26th March, 2014
advertisement

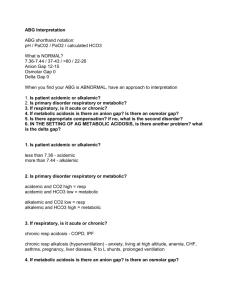
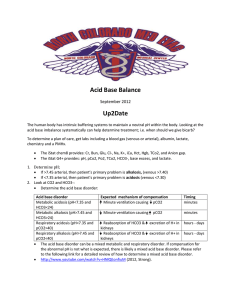
OSCE 26th March, 2014 Case 1 67 years old gentleman attended AED after a fall at escalator. He complained of neck pain afterwards. He did not have any limb weakness or sphincter disturbance What are the abnormalities? Fracture dens of C2 Degenerative changes with post nipping of the osteophytes in C4/C5, C5/C6 How to classify the pathology? Dens fractures are classified as type I, II, or III. Which ligamental injury is associated with this condition. Transvere alantal ligament Transverse atlantal ligament disruption occurs in approximately 10% of cases. Injuries of this ligament can result in atlantoaxial instability after odontoid fracture osseous healing, and the chance of odontoid fracture non-union is increased with its disruption. Give 2 complication of this condition nonunion malunion pseudoarthrosis formation infection neurovascular injury acute airway compromise Treatment modalities: externally immobilized by a halo vest fused surgically. Case 2 73 years old gentlemen had history of hypertension and diabetes. He presented to our department with dizziness, sweating and urinary incontinence. He had fever and coryzal symptoms few days ago and had consulted private doctor Describe the ECG SR 90/min ST elevation V1-V2 Negative T V1-V2 On further asking, this patient had history of recurrent syncope few years ago. By that time investigation was normal. What will be your diagnosis? Brugada syndrome Type1 Type 2 Type 3 What test will you order to confirm your diagnosis? Flecainide stress test/ Stress test with Class 1a, 1c or Class III drugs What will be the treatment? Implantable cardioverter defibrillator (ICD) Case 3 61 years old gentleman presented with acute dysphagia. He had history of foreign body (fishbone) ingestion 2 days ago Describe the findings Rim enhancing collection noted along the left oropharyngeal space What is your diagnosis? Left retropharyngeal abscess Relations of the retropharyngeal space: * Superior: Base of the skull * Inferior: Superior mediastinum * Lateral: Carotid sheath * Anterior: Buccopharyngeal fascia * Posterior: Alar fascia What is the common causative organism? Aerobic organisms, such as beta-hemolytic streptococci and Staphylococcus aureus Anaerobic organisms, such as species of Bacteroides and Veillonella Gram-negative organisms, such as Haemophilus parainfluenzae and Bartonella henselae Name 2 complications of this disease Airway obstruction. Mediastinitis. Pericarditis. Aspiration pneumonia. Epidural abscess. Septicaemia. Adult respiratory distress syndrome(ARDS). Case 4 70 years old gentleman had history of malignancy, just put on chemotherapy few days ago. He presented to AED with poor oral feeding, repeated vomiting and dizziness. BP was 92/62, pulse 130/min at triage. What is your differential diagnosis? Hypovolaemic shock (GI loss) Distributive shock (septic shock) Obstructive shock ( Cardiac tamponade, pulmonary embolism) Cardiogenic shock (ACS) What is your diagnosis? Cardiac tamponade What will the likely cause and the treatment? Malignancy Pericardiocentesis What is the bedside investigation to confirm your diagnosis? Cardiac ultrasound/ Echocardiogarm What will be the diagnostic finding in that investigation? Pericardial effusion with RA/RV diastolic collapse Case 5 62 years old gentleman presented to AED with repeated vomiting and diarrhoea. He had returned from Saban 2 days ago and had taken seafood there. The serum Na on admission is 118. He was put on normal saline and admitted EMW. On next day Na dropped to 108. Urea 2.9, Cr 64. Blood pressure was normal. Hydration was good and there was no edema. Name 3 possible causes of the hyponatraemia. SIADH Hypothyroidism Addision’s disease Pseudohypontraemia Fluid loss Hyponatraemia Isovolemic: SIADH, hypothyroidism, Addison’s disease, water intoxification Hypovolemia: Fluid loss, dehydration, diuretics, adrenal insufficiency Hypervolemic: CHF, cirrhosis, CRF Name 3 laboratory investigations you will perform. Urine Na Serum/ urine osmolality TFT Spot cortisol Synathen test The serum osmolality is 240mOsmol/kg and urine Osmolality is 567mOsmol/kg. What is your diagnosis? SIADH What will be your treatment? Fluid restriction Sodium supplement In symptomatic hyponatraemia, what kind of fluid should be given and what will be the maximal rate of increase of sodium per hour? Hypertonic saline (3% or 5.85% NaCl solution) Maximal rate 0.5mM/hr elevation What is the risk of rapid rise of sodium level? Central pontine myelinolysis Case 6 A 20 year-old lady with known history of asthma on regular puffs presented to your ED for acute dyspnea in the middle of the night. Here are her vital signs Conscious, however apprehensive BP 130/80, pulse 130/min SpO2 98% on 4L/min O2 via nasal cannula Talk in phases Temperature 38 degree Celsius What investigations would you do/order in ED? ABG (i-stat or point of care test) Peak expiratory flow rate, PEFR CXR ECG CBP D/C, R/LFT, Clotting profile Here is her blood gas, please interpret pH 7.28 pCO2 41.25mmHg pO2 80mmHg HCO3 20 BE -4 Na 128 K 4.0 Chloride 85 High anion gap metabolic acidosis, respiratory acidosis together with metabolic alkalosis pH 7.28 --> Acidosis HCO3 20, BE -4, --> metabolic acidosis Expected PaCO2 28mmHg +/- 2, however now is 41.25mmHg --> respiratory acidosis Anion gap 27 --> High anion gap metabolic acidosis Delta anion gap 15, delta HCO3 4, Delta anion gap/Delta HCO3 ( Delta ratio ) = 3.75 >2 therefore metabolic alkalosis What is your initial management in ED? Oxygen supplement with continuous SpO2 monitoring Puff bronchodilator including Ventolin/Atrovent, no ceiling dose IV steroid, hydrocortisone 100mg-200mg stat MgSO4, 10mmol loading within 10-30minutes Prepare for intubation with mechanical ventilation, in selected case, may have a trial of non-invasive ventilation Consult ICU She deteriorates further and you decide to intubate her, what medications will you give for your RSI? Induction agent: Ketamine / Propofol Muscle relaxant: Suxamethonium Avoid giving histamine releasing medications including morphine After your intubation, your portable ventilator alarms and there is essentially no tidal volume achieved. Why? Bronchospasm with high airway pressure as a result of high airway resistance that exceed the upper pressure limit Pneumothorax Your ICU colleague agree to admit the patient but has to wait for 30 minutes in your resuscitation room, they can borrow a conventional ventilator for you, what is your initial setting of the ventilator? Sedate and paralyze the patient SIMV(VC) + PS TV 6ml/kg predicted body weight Zero PEEP FiO2 1.0 RR 8-10/min, adjusted according to the flow-time or volume-time curve Prolonged IE ratio e.g. 1:3.3 to 1:10 Increase the peak airway pressure limit to for example 100 Measure iPEEP and Plateau pressure Thank you