Assessment of the Pulmonary System
advertisement
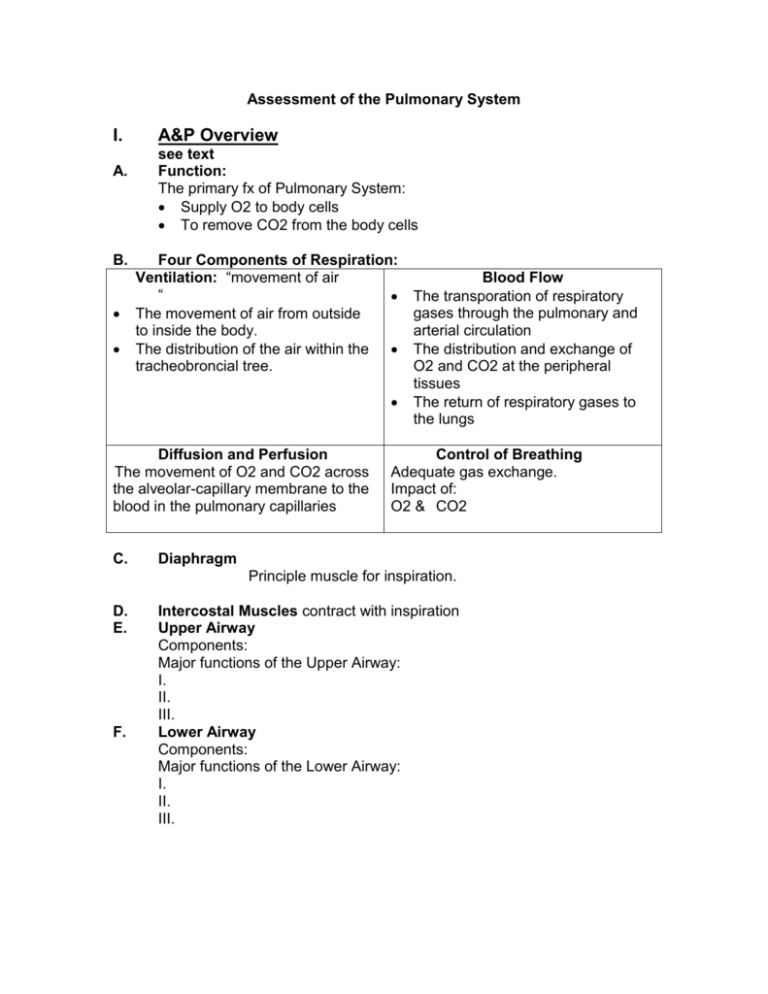
Assessment of the Pulmonary System I. A. B. A&P Overview see text Function: The primary fx of Pulmonary System: Supply O2 to body cells To remove CO2 from the body cells Four Components of Respiration: Ventilation: “movement of air “ The movement of air from outside to inside the body. The distribution of the air within the tracheobroncial tree. The Diffusion and Perfusion The movement of O2 and CO2 across the alveolar-capillary membrane to the blood in the pulmonary capillaries C. Blood Flow The transporation of respiratory gases through the pulmonary and arterial circulation The distribution and exchange of O2 and CO2 at the peripheral tissues The return of respiratory gases to the lungs Control of Breathing Adequate gas exchange. Impact of: O2 & CO2 Diaphragm Principle muscle for inspiration. D. E. F. Intercostal Muscles contract with inspiration Upper Airway Components: Major functions of the Upper Airway: I. II. III. Lower Airway Components: Major functions of the Lower Airway: I. II. III. G. Landmarks of the Thorax Anterior Thorax 1. Clavicle: The apex of the lung rises approx 3-4 cm above ea clavicle 2. Suprasternal Notch: The depression just above the sternum 3. Sternum: divided into three segments A. Manubrium (Upper) B. Body of Sternum (Middle) C. Xiphoid Process (Lower) 4. Angle of Louis (Manubriosternal angle) 5. Coastal Angle: 6. Intercostal space: Posterior Thorax 1. Vertebra Prominens 2. Spinous Processes 3. Inferior Border of the Scapula Reference Lines Anterior Mid-sternal Mid-clavicular II. Axillary Anterior axillary Mid-axillary Posterior axillary Posterior Scapular Line Vertebral Line Assessment of the Respiratory System A. History 1. Coughing: could be r/t: Symptom analysis: Duration: 1. How long have you had the cough? 2. How long does ea episode last? Frequency How often does it occur? Once/day, week, hr? Circumstances What causes? Activity? Time of day, Position (lying down at night? Sitting?) Talking? Exercise/activity How affects? Does the cough interfere with activities? How much activity precipitates? (Walking 5 feet? Walking 10 feet or more) History Personal history of allergies? Family hx allergies? Respiratory problems? Smoking hx (personal, does anyone in the household smoke?) Self-care 1. What helps? Sitting, standing, lying down…. 2. What have you done to treat? (specifics re: medications/ treatments (warm shower, lemon tea, etc). Exacerbation/Improvement Perceptions re: whether the cough is improving or getting worse. The pt should define “worse” for himself. Other: Type of cough (Dry, hacky, bubbling, barking, congested) Sputum production (Describe:1. amt 2. Consistency 3. Color 2. Shortness of Breath or Dyspnea on Exertion; Difficulty Breathing or Breathlessness Symptom analysis: Symptom analysis: Duration: Frequency Circumstances Exercise/activity History Self-care Exacerbation/Improvement Other: 3. B. Miscellaneous History a. Previous hx respiratory illness, hospitalization, surgeries b. Date of last Chest X-ray c. Currently taking any medications d. Environmental factors: Fumes, chemicals, insecticides, place of employment, use of air freshenors e. Smoking hx: What How long? How much/day Does he inhale Does he have a cough which seems to be asso with smoking Does he have the desire to quit smoking? Preparation for Exam 1. Position of Client 2. Sequence: Inspection of the thorax Palpation, Percussion, Auscultation of anterior thorax Palpation, Percussion, Auscultation of the posterior thorax 3. Clothing: 4. Odor) C. Physical Exam of the Thorax 1. Inspection a. Breathing Pattern Men: Women: Terms: Tachypnea Bradypnea Kussmaul’ s Biot Breathing CheyneStokes Terms to Know Definition “Normal” occurance Resp. rate greater than Fear, anxiety, 24/min. exercise Resp rate less than 12/min Breathing pattern that involves increased rate and depth of respirations. Breathing pattern that involves shallow breathing for 3-4 breaths, followed by a period of apnea. Breathing pattern that involves a period of rapid rate respirations followed by normal/slower respirations. What would be abnormal? Use of accessory muscles to breath Supraclavicular retractions Intercostal retractions Intercostal bulging b. Nailbeds Bluish discoloration suggests: Clubbing suggests: c. Chest wall configuration d. Anterior posterior diameter Potential Pathology Fever, Pulmonary pathology Drug induced; Increased intracranial pressure Diabetic Ketoacidosis e. Level of Consciousness 2. Assessment of the Posterior Chest a. Assessment of Respiratory Excursion of the Posterior Chest Procedure: b. Assessment of Tactile Fremitus over the Posterior Chest Procedure: Abnormalities: c. d. Palpation of the Skin of the Posterior Chest Note: Tenderness Skin temp Moisture Superficial lumps or masses Crepitus (subcutaneous emphysema). Percussion of the Posterior Chest Position . Procedure: Findings:. Tones: Resonance: Dullness: Tympany: Abnormalities: e. Diaphragmatic excursion Tape reviews – this is a method used to determine the size of the diaphragm. We will not do in lab – but notice how it is done. f. Auscultation of the Posterior Thorax Position: Procedure: Sound Bronchial Bronchovesicular Vesicular Respiratory sounds: Normal Location Trachea, larynx Major bronchi (where there are no alveoli): Between scapula, around the sternum Peripheral lung Description Expiration is the loudest, longest sound. Loud, harsh sound. Inspiration = Expiration Moderate pitch. Inspiration is loudest and longest. Soft, rustling sound. Like the sound of the wind. Air is flowing through the smaller bronchioles and alveoli. Abnormalities: Decreased/absent breath sounds Silent chest Increased breath sounds Abnormal Breath Sounds: Crackles (Rales): Rhonchi: Wheeze: . Documentation of abnormal breath sounds. Must include: Sound heard (crackles, rhonchi, wheeze), location of sound (Right upper chest, Left Lower Lobe, etc.), respiratory phase (Inspiration, Expiaration, both), does coughing improve? g. 3. Vocal Resonance/Whispered Pectoriloquy You will see on video – we will not cover in lab/exam. Assessment of the Anterior Chest a. Assessment of Respiratory excursion of the Anterior Chest b. Assessment of Vocal Fremitus of the Anterior Chest c. Percussion of the Anterior Chest d. Auscultation of the Anterior Chest D. Considerations with Infants and Children Encourage parent participation. Parents can hold during exam. If asleep – take advantage of opportunity to inspect, auscultate, palpate, percuss. Crying enhances tactile fremitus Play with the child Infants have a rounder thorax, by age 6 it should be 1:2 Infants are nose breathers until the age of 3 months. E. Considerations with the Elderly Increased anterior/posterior diameter Kyphosis (outward curve of the spine) Slight decrease in chest expansion (what does this mean?) Note that it should remain symmetrical.