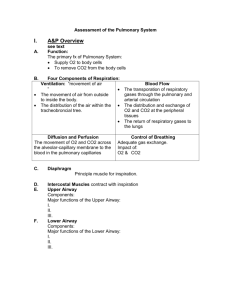
RESPIRATORY EXAMINATION
advertisement

RESPIRATORY EXAMINATION Positioning the Patient ∙ ∙ The patient should be undressed with the breasts (if female) and genitals covered. If the patient is not acutely ill they should be asked to sit on the edge of the bed. If they are unwell the bed should be positioned so that they can sit back as vertically as possible. General Appearance ∙ The general rule in examining patients’ respiratory system is that the major findings will be found from the back. There are a number of important findings that can be found when examining patients anteriorly which may be useful before proceeding to patients’ backs, however this initial examination from the front should not waste too much time because most findings will be found at the back. ∙ With this in mind, begin the examination by sitting on a chair in front of the patient or by standing in front of them to facilitate general inspection. You may wish to hold their hands. Look for: 1. Hoarseness of voice: Recurrent laryngeal nerve palsy, laryngitis. 2. Tachypnoea (>14 breaths per minute). Count the breaths for 30 seconds. (Many of the following observations can be made while counting the respiratory rate.) 3. Dyspnoea and Accessory muscle use: sternomastoids, platysma, tracheal tug or intercostal recession. 4. Oxygen therapy and intravenous medications. 5. Audible wheeze: Ask the patient to have a few deep breaths in-an-out through their mouth. 6. Stridor: Ask the patient to have a few deep breaths in-an-out through their mouth. 7. Cough: Ask the patient to cough. A soft, prolonged “bovine” cough may indicate vocal cord paralysis. Cough may also be productive, dry or wheezy. 8. Sputum: Ask to see the patient’s sputum cup. 9. Vital signs: Ask to see the chart or ask for the temperature, BP and urinalysis. 10. Cyanosis: Check for central cyanosis by asking the patient to poke their tongue out (occurs with SaO2 <90%). 11. Inspection of the anterior chest wall: - pectus carinatum - pectus excavatum - scars - kyphoscoliosis - radiotherapy tattoos or burns - SVC obstruction Hands 1. Tar staining. 2. Wasting of the small muscles of hand,: may occur with lower brachial plexus (C8, T1) lesion due to infiltration/compression by lung tumour (Pancoast’s tumour). 3. Clubbing . To detect clubbing: - 687292521\5/02/2016 Observe the angle between the nail bed and the base of the finger (the unguophalangeal angle). This should be less than 180; Ballott the nail bed by pressing the distal nail with a finger of one hand while holding a finger of the other hand over the proximal nail. A “floating” nail will rise up through spongy, soft tissue; 1/4 - - - Observe the distal phalanx for the characteristic “drumstick” shape; Clubbing may occur with respiratory disease (carcinoma, suppurative lung disease, idiopathic pulmonary fibrosis, asbestosis and cystic fibrosis) mediastinal disease (e.g. thymoma or lymphoma), cardiovascular disease (SBE, cyanotic congenital heart disease) and other disease (e.g. cirrhosis, coeliac disease, inflammatory bowel disease, thyrotoxicosis, pregnancy, familial and idiopathic). unilateral clubbing may occur with aortic or subclavian aneurysm, axillary tumour, Pancoast’s syndrome, lymphangitis, apical TB, ulnar neuritis, post-trauma, sarcoidosis and tophaceous gout. clubbing does not occur with CAL. Hypertophic Pulmonary Osteoarthropathy (HPO) – In patients who have clubbing, this may be assessed by squeezing distal radius/ulna, wrists and metacarpals for tenderness and swelling due to periosteal inflammation. Occurs as a paraneoplastic phenomena with lung carcinoma and mesothelioma. This should only be done in those with clubbing, not routinely otherwise. 4. Trachea ∙ Standing in front of the patient gently push the middle finger (3rd finger) of the right hand into the suprasternal notch with the index finger and ring finger on either side. The middle of the trachea should be felt at the end of the middle finger. This is one of the more important findings that you will find if you examine the patient from the front. The reason is that lesions which pull the trachea towards them have a different etiology than those that push them away. When you proceed to examine the rest of the lungs , you will be able to make this distinction clearly. (So, for example, if there is dullness at the right upper zone, and the trachea deviates to the right, the etiology will be likely to be entirely different to if there is dullness at the right upper zone and the trachea deviates to the left.) ∙ ∙ Deviation to side of lesion: Upper lobe collapse, upper lobe fibrosis, pneumonectomy. Deviation away from lesion: Tension pneumothorax, massive effusion. Chest ∙ When examining the chest start posteriorly as this examination is easier and generally more informative than examination of the anterior thorax. All modalities of examination should be done on the posterior thorax and in the axillary region (palpation, percussion, auscultation) before examining the anterior thorax. Inspection 1. Chest Wall movement Upper lobe expansion is best assessed by standing behind the patient and looking down at the clavicles during normal respiration. Lower lobe expansion is best assessed by looking at the entire posterior thorax. Unilateral reduction occurs with consolidation, pleural effusion, collapse or pneumothorax. Bilateral reduction occurs with CAL or pulmonary fibrosis. 2. Scars - 687292521\5/02/2016 surgery radiotherapy changes 2/4 Palpation 1. Chest Expansion (Lower lobe) ∙ Place your hands on the chest wall with the fingers extended around the sides of the chest. Your thumbs should meet in the midline but be held off the chest to allow movement with respiration. Test on full inspiration and expiration. Should be >5cm. Observe for unilateral or bilateral reduction. (It should be noted that this is a very unreliable sign, as it is possible to markedly affect one’s respiratory excursions by voluntary effort. The student can demonstrate this by breathing first with just the upper part of the chest, then with only the lower part of the chest. The most important sign is not increase or decrease in chest excursion, rather it is assymettry of chest excursion. Some authors also recommend feeling for the strength of chest excursion, rather than looking at the distance of chest excursion, as this is thought to be more reliable) 2. Tactile Fremitus ∙ ∙ Palpate both sides of the chest wall with the palm of each hand as the patient repeats “ninety-nine” or “toy boat”. Significance is the same as vocal resonance but it is generally less sensitive. Because of this, it is probably only necessary to do vocal fremitus or vocal resonance (preferably vocal resonance), not both. Percussion ∙ ∙ Percuss symmetrical areas of the posterior and axillary regions. Always compare one side with the other. Ask the patient to place their hands on their head or to cross their arms to facilitate examination of the axillary region. Percussion note may be recorded as normal, hyperresonant, dull and (occasionally), “stony” dull. Auscultation ∙ ∙ Listen over each area of the lung - always comparing one side with the other. Note: 1. Quality of breath sounds: vesicular (normal); bronchial: consolidation, above pleural effusion, collapse, localised fibrosis, large cavity. 2. Intensity record as normal, reduced or absent breath sounds. reduced with CAL, effusion, pneumothorax, consolidation, collapse. 3. Added sounds wheeze due to airflow obstruction; crackles due to abrupt opening and collapse of distal airways. May describe timing and character of crackles a. Early inspiratory: medium (CAL). b. Late or pan-inspiratory: fine (pulmonary fibrosis), medium (LVF) and coarse (bronchiectasis). pleural friction rub: pneumonia, infarct, pleural malignancy, pneumothorax. 4. Vocal resonance: Ask the patient to say “ninety-nine”, “Nadi” or “toy boat” and listen to both sides of the chest noting any asymmetry. increased in areas of consolidation. may hear “whispering pectoriloquy” if prominent consolidation. 687292521\5/02/2016 3/4 Note: ∙ When examining the anterior thorax: - percuss the upper lobes by percussing the clavicle directly. - auscultate the upper lobes by using the bell in the supraclavicular fossa. Neck (This may be better examined between moving from the posterior chest back to the anterior chest) - Lymphadenopathy - occipital - pre and post-ouricular - submandibular and submental - cervical (anterior and posterior) - supraclavicular axillary lymphadenopathy (may be examined at the completion of the examination). Face (These signs are rarely found and should be only searched for if they are likely to be relevant to the rest of the overall picture.) 1. Eyes - Horner’s Syndrome (meiosis, ptosis, anhydrosis) 2. Nose - polyps (with asthma) 3. Mouth - tongue (central cyanosis) - dentition (source of bacterial infection) Relevant Cardiac Examination ∙ 1. 2. 3. 4. 5. 6. 7. 8. 9. After examining the anterior thorax, reposition the patient at 45 and perform a directed cardiac examination. Palpate the apex beat. Right ventricular heave: Examine by bending down and looking across the sternum, and then palpating for a heave. Palpate for a palpable pulmonary valve closure. Observe the JVP. Auscultate the heart briefly: Take particular notice of any added sounds e.g. S3, split S2 or murmurs or features of pulmonary hypertension. Axillary lymph nodes. Feet. Examine for pitting oedema (which may be a sign of cor pulmonale). Examine the abdomen for a ptosed liver or features of malignancy. Consider examination of other systems e.g. breasts, skin, abdomen, lymph nodes, rectum - for features of primary or secondary malignancy. 687292521\5/02/2016 4/4