surgery respiratory
advertisement
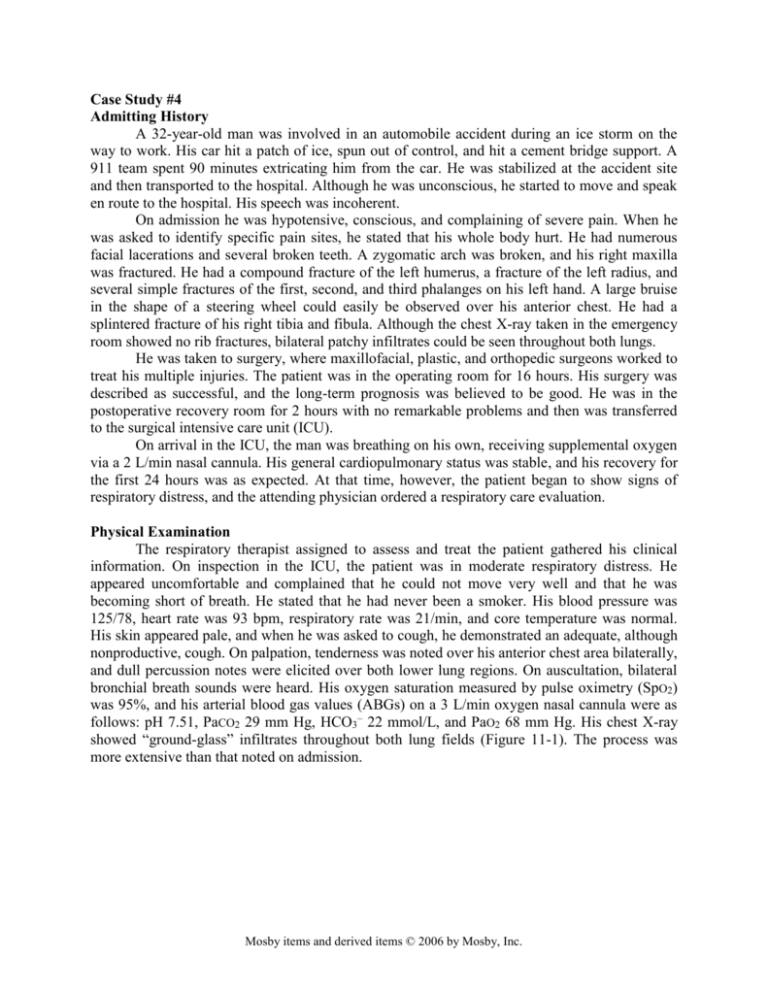
Case Study #4 Admitting History A 32-year-old man was involved in an automobile accident during an ice storm on the way to work. His car hit a patch of ice, spun out of control, and hit a cement bridge support. A 911 team spent 90 minutes extricating him from the car. He was stabilized at the accident site and then transported to the hospital. Although he was unconscious, he started to move and speak en route to the hospital. His speech was incoherent. On admission he was hypotensive, conscious, and complaining of severe pain. When he was asked to identify specific pain sites, he stated that his whole body hurt. He had numerous facial lacerations and several broken teeth. A zygomatic arch was broken, and his right maxilla was fractured. He had a compound fracture of the left humerus, a fracture of the left radius, and several simple fractures of the first, second, and third phalanges on his left hand. A large bruise in the shape of a steering wheel could easily be observed over his anterior chest. He had a splintered fracture of his right tibia and fibula. Although the chest X-ray taken in the emergency room showed no rib fractures, bilateral patchy infiltrates could be seen throughout both lungs. He was taken to surgery, where maxillofacial, plastic, and orthopedic surgeons worked to treat his multiple injuries. The patient was in the operating room for 16 hours. His surgery was described as successful, and the long-term prognosis was believed to be good. He was in the postoperative recovery room for 2 hours with no remarkable problems and then was transferred to the surgical intensive care unit (ICU). On arrival in the ICU, the man was breathing on his own, receiving supplemental oxygen via a 2 L/min nasal cannula. His general cardiopulmonary status was stable, and his recovery for the first 24 hours was as expected. At that time, however, the patient began to show signs of respiratory distress, and the attending physician ordered a respiratory care evaluation. Physical Examination The respiratory therapist assigned to assess and treat the patient gathered his clinical information. On inspection in the ICU, the patient was in moderate respiratory distress. He appeared uncomfortable and complained that he could not move very well and that he was becoming short of breath. He stated that he had never been a smoker. His blood pressure was 125/78, heart rate was 93 bpm, respiratory rate was 21/min, and core temperature was normal. His skin appeared pale, and when he was asked to cough, he demonstrated an adequate, although nonproductive, cough. On palpation, tenderness was noted over his anterior chest area bilaterally, and dull percussion notes were elicited over both lower lung regions. On auscultation, bilateral bronchial breath sounds were heard. His oxygen saturation measured by pulse oximetry (SpO2) was 95%, and his arterial blood gas values (ABGs) on a 3 L/min oxygen nasal cannula were as follows: pH 7.51, PaCO2 29 mm Hg, HCO3– 22 mmol/L, and PaO2 68 mm Hg. His chest X-ray showed “ground-glass” infiltrates throughout both lung fields (Figure 11-1). The process was more extensive than that noted on admission. Mosby items and derived items © 2006 by Mosby, Inc. Case Study Figure 11-1 2 Chest X-ray of a 32-year-old man with 1. Which pulmonary conditions are associated with trauma? 2. What disease process should the team suspect that he has? 3. What evidence supports it? 4. What other disease processes could occur secondary or along with this one? 5. What is the interpretation of the current blood gas? Why? 6. What are some immediate actions that he RCP could take? 7. What are some treatment recommendations that the RCP could make? 3 Days After Surgery The patient paged the nurse and stated that he was feeling worse. Respiratory care was called. The patient appeared cyanotic on observation. His respiratory rate was 30/min, blood pressure was 165/95, heart rate was 110 bpm, and rectal temperature was 38.8° C (101.8° F). His cough was still nonproductive, and his anterior chest was still tender. Bronchial breath sounds and crackles were heard throughout both lung fields. His SpO2 was 75%, and his ABGs were as follows: pH 7.56, PaCO2 24 mm Hg, HCO3– 18 mmol/L, and PaO2 35 mm Hg. No recent chest Xray was available, but one had been ordered. 1. Is the pt in respiratory distress? 2. What evidence supports it? 3. What is the interpretation of the current blood gas? Why? 4. What are some immediate actions that he RCP could take? 5. What are treatment recommendations that the RCP could make? 6. What can be used to determine if the disease process has worsened? Mosby items and derived items © 2006 by Mosby, Inc. Case Study 3 30 Minutes Later The respiratory therapist assigned to monitor and evaluate the patient noted that the patient’s respiratory rate was 18/min, blood pressure was 170/97, heart rate was 150 bpm, and rectal temperature was 37.8° C (100° F). He appeared cyanotic, and no longer responded verbally when asked questions. On auscultation, bronchial breath sounds and crackles could be heard bilaterally. His SpO2 was 69%, and his ABGs were as follows: pH 7.31, PaCO2 48 mm Hg, HCO3– 22 mmol/L, and PaO2 31 mm Hg. A current chest X-ray showed increased opacities throughout both lung fields. 1. 2. 3. 4. What is the interpretation of the patient’s condition? What is the ABG interpretation? Why? What immediate action should be taken by the healthcare team? Why? If this patient becomes intubated, how should he be ventilated? Mosby items and derived items © 2006 by Mosby, Inc.