Gastro06-IntroGIRadiologicImaging
advertisement

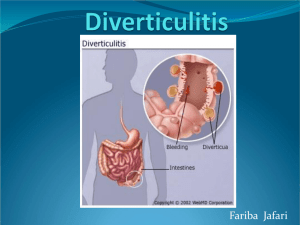
GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 1 of 6 Introduction to Radiologic Imaging of the GI System Note: This scribe is basically the same as found in pages 40-47 of our syllabus and it follows along w/ the 32 images posted online by Dr. Sharratt. Also, Dr. Sharratt was gracious enough and went over the test material in the first 5 mins. of class which I have bolded in this scribe. He said that these items were verbatim test questions from him. ABDOMEN: Esophagus, Stomach, Small Bowel, and Colon I. - ESOPHAGUS Reflux esophagitis: (Slide #1) Double-contrast esophagram in a patient with a sliding hiatal hernia demonstrates effacement of linear folds and shallow ulcerations typical of reflux esophagitis. Barrett's esophagus and hiatal hernia: (Slide #2) This middle-aged man had a long history of dyspepsia and heart burn. Spot film of the esophagus from a double-contrast upper GI series shows a sliding hiatal hernia. Note the "filigree" pattern -- fine reticular collections of barium between slightly elevated mucosal folds in the distal esophagus, resembling the areae gastricae. Example of a Barrett's esophagus. COMMENT: Barrett's esophagus is generally considered an acquired disorder. Radiograph reflects the presence of columnar acid secreting gastric mucosa, now present within the distal esophagus. Stricture formation may be a common sequela. You’ll see cases of squamous cell carcinoma being most common → mid-esophagus. This may also undergo adenocarcinomatous degeneration – distal 1/3 of esophagus – which is associated w/ Barrett’s esophagus. Barrett’s esophagus is associated w/ gastroesophageal reflux. Sliding hiatal hernia with Schatzki's ring: (Slide #3) This spot film shows small hiatus hernia. Numerous gastric mucosal folds extend through the hiatus and to the prolapsed stomach. The esophagogastric junction is marked by a well-defined symmetrical ring that measures 2 to 3 millimeters in height (Schatzki ring). A Schatzki ring is seen in significant percentage of patients with hiatus hernia. It marks the squamocolumnar junction and therefore indicates the position of the esophagogastric junction. Achalasia is another of the motility disorders. In this instance, there is a failure of relaxation of the cardia resulting in retention of food, saliva, and secretions in the esophagus. (Slide #4) This 49-year-old man complained of progressive dysphagia for approximately two years. On the left, an erect delayed film of an esophagram shows a large dilated esophagus. Retained secretions are layered above the barium. There is a small amount of barium within the stomach. The film on the right reveals the esophagogastric junction to be a long narrowed segment with an intact mucosa. This appearance is characteristic of achalasia. Esophageal varices: The serpiginous filling defects in the distal third of the esophagus represent esophageal varices. They changed slightly in contour and size during the fluoroscopic examination. (Slide #5 ) Bleed like crazy. Esophageal infections are unusual. When they do occur, they are usually a result of opportunistic invaders such as Candida, herpes simplex virus, or Cytomegalovirus. They almost always occur in debilitated or immunosuppressed patients. (Slide #6) These three images are examples of Candida esophagitis in three different patients with AIDS. The upper left-hand corner is a double-contrast esophagram revealing a coarse mucosa with shallow ulcerations. The upper right-hand corner radiograph shows replacement of the normal mucosal pattern of coarse thickened mucosa. The lower left-hand radiograph is a spot film of the mid esophagus in a third patient showing an elongated deep ulcer. The findings were confirmed at endoscopy in all three patients. GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 2 of 6 COMMENT: The radiologic findings in Candida esophagitis vary with the degree of invasiveness. The earliest radiologic manifestation is a fine mucosal irregularity which can be appreciated on doublecontrast studies. Unfortunately, many patients have severe odynophagia and they may not be able to tolerate a double-contrast examination. In patients with more extensive mucosal colonization, superficial plaques and nodules may be seen radiographically. Spasm is frequently identified. Focal ulceration and intraluminal masses may be seen in a small percentage of cases. Strictures may develop with healing. These strictures may mimic the radiographic appearance of strictures that develop following ingestion of corrosives. Herpetic and Cytomegalovirus infections usually result in ulcerations of the esophageal mucosa. Herpetic ulcerations are small well defined and aphthoid in appearance. Cytomegalovirus ulcers may be large and extend over several centimeters. This and the following are representative examples of carcinoma of the esophagus. On this slide (Slide #7) this elderly patient complained of progressive dysphagia and epigastric pain. The esophagram on the left demonstrates an eccentric narrowing of the distal esophagus with an overhanging edge at the proximal margin of the narrowed segment. The CT scan on the right demonstrates a filling defect in the cardia which represents a large gastric metastasis. This 70-year-old woman (slide #8) complained of progressive dysphagia for solid foods and a thirty-pound weight loss over a three-week period. The esophagram on the left demonstrates a narrowed segment of the mid and distal esophagus with mucosal destruction. Note the overhanging edges at the proximal margin of the lesion. The CT examination on your right was obtained at the level of the carina. This reveals tumors surrounding the markedly narrowed esophageal lumen which contains a small amount of air and contrast material. Note compression of the carina and left main stem bronchus. No fat plane is seen between the mass and the aorta. Endoscopic biopsy reveals squamous cell carcinoma. COMMENT: Most esophageal carcinomas appear in the middle third of the esophagus. The distal third, particularly the region of the gastroesophageal junction, is the next most common site, while the proximal esophagus is the least common site of this tumor. The differential diagnosis of esophageal carcinoma includes achalasia, benign stricture, and Crohn's disease. Not all filling defects of the esophagus are so ominous. This young man (slide #9) complained of dysphagia for solids. As a child, he had undergone several esophageal dilatations for a corrosive stricture. These two slides reveal a 2-centimeter intraluminal filling defect at the junction of the middle and distal thirds of the esophagus. There is a narrowing of the distal third of the esophagus with evidence of partial obstruction (note the fluid level). Further history revealed that the patient was a drug dealer who concealed his drugs in a balloon that he swallowed when police approached and regurgitated when they left. II. - STOMACH Developmental abnormalities encountered in the adult are not common to begin with. The two that occur with any frequency, are gastric duplications and prepyloric antral webs. Gastric duplication: (slide #10) These two radiographs, supine and erect views of a double contrast study, show a large sharply demarcated submucosal mass projecting into the gastric lumen. Note the effacement of the overlying mucosa. Operation revealed a duplication cyst. Prepyloric antral web: (slide #11) This 63-year-old man complained of episodic, epigastric distress and intermittent vomiting. The uppermost image is from a double contrast spot film; the lower is from a singlecontrast spot film. Note a band-like linear defect with a 1-centimeter central aperture in the antral portion of the stomach. The location, about 1.5 centimeters proximal to the pyloric channel, is typical of both congenital (usually) and acquired antral webs → most acquired through scarring from PUD. COMMENT: Prepyloric antral webs (also known as diaphragms or membranes) are encountered mainly in two age groups: young infants and the middle-aged (fifth and sixth decades). Antral webs found in infants are presumably of developmental origin; while congenital webs undoubtedly occur in adults, the GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 3 of 6 great majority of duodenal webs detected after childhood are probably related to peptic ulcer disease. Gastric outlet obstruction may occur in chronic or untreated cases. The typical radiologic features of a benign gastric ulcer include the following: 1) projection of the barium-filled crater beyond the gastric lumen, 2) mucosal folds radiated to the margin of the ulcer, 3) a fine 1 - 2 mm collar at the neck of the ulcer (Hampton's line). Spasm is a common associated finding. (Slide #12) These two images exemplify a benign gastric ulcer. The one on the left reveals the ulcer in profile. The ulcer has a long neck and a surrounding inflammatory mound. On the right is an en face view revealing effacement of the rugal folds in the vicinity of the crater. The diagnosis of benign gastric ulcer was confirmed by endoscopy. Ulcers have to be Bx to tell if benign or malignant. Gastric neoplasms may be benign or malignant. Benign gastric tumors may be classified into two broad morphologic groups: 1) mucosal (polypoid), 2) submucosal. Mucosal benign neoplasm: Most common of the benign gastric neoplasms is the benign gastric polyp occurring in 1 - 2% of the adult population. These are best demonstrated by the double-contrast technique. Approximately 50% of the patients with gastric polyps have more than one. (Slide #13) As can be seen on this study, this 66-year-old woman had multiple polyps. The arrows point to prolapse of one of these polyps through an anastomotic junction between the stomach remnant and the jejunum. This is evidence of the patient's prior history of a Billroth II type of gastrectomy. A Billroth II gastrectomy is an antrectomy with an antecolic end to side gastrojejunostomy. (A Billroth I gastrectomy is commonly used in North America to describe a partial gastrectomy (Antrectomy) with gastroduodenostomy. The procedure may be end to end or end to side or side to side with a superior, inferior, posterior, or anterior anastamosis. Submucosal: Submucosal lesions may be leiomyomas, lipomas, neurofibromas, carcinoid, hemangioma, myoblastoma, and hemangiopericytoma. (Slide #14) The study above reveals a prolapsing antral lipoma. This 53-year-old woman had an upper GI series as part of a staging work-up for carcinoma of the cervix. She had no gastrointestinal complaints. The four slides above are sequential spot films showing an oval 4 cm mass extending from the antrum into the duodenum. The mass has a smooth sharply defined border and exhibits changeability from film to film. The CT scan below shows a well- defined intraluminal filling defect in the antroduodenal region. (Slide #15) The CT number was -57 hu., consistent with fat (lipoma). Malignant neoplasms of the stomach are the 7th leading cause of cancer deaths in the United States. There is an incidence of approximately 8 per 100,000. Gastric carcinomas generally arise in the distal portion of an otherwise normal stomach. Gastric carcinoma typically metastasizes to the liver and to regional lymph nodes. Scirrhous carcinoma may spread submucosally extending to the pylorus or esophagus. This is representative of the superficial spreading type of gastric cancer. (Slide #16) This 68-year-old man presented with dysphagia. Both spot films of the Upper GI series show grossly thickened antral folds. Note the changeable contour of the affected segment. There was no delay in gastric emptying. A partial gastrectomy was performed. Pathological examination revealed a moderately differentiated adenocarcinoma involving the mucosa and submucosa. Tumor was present in the lymphatics and regional lymph nodes (bad news). (Slide #17) This middle-aged man presented with dyspepsia and weight loss. A prone oblique view of the stomach shows a 6-centimeter fixed polypoid lesion on the greater curvature of the stomach. The CT examinations shown to the right are adjacent slices and show both the mural (arrows in the more superior image) and intraluminal (arrows in the lower CT scan) components of the neoplasm. GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 4 of 6 III. - DUODENUM - inch for inch, one of the most common Peptic ulceration of the duodenum represents a wide range of radiologic appearances. A small duodenal ulcer may have the appearance of an ulcer crater as seen above. (Slide #18) This is a supine film from an upper GI series revealing a half-centimeter collection of barium within a centrally located posterior wall ulcer. The duodenal bulb is not deformed. The failure to demonstrate an ulcer crater does not exclude active disease in patients with a typical clover leaf deformity as seen above. This is a common finding in patients with severe peptic ulceration in which there is scarring and spasm of the duodenal cap. COMMENT: Time constraints preclude further discussion of both benign and malignant pathology that may be found in this short segment of small bowel known as the duodenum. Suffice it to say that inch for inch the duodenum is one of the most common sites of malignancy in the gastrointestinal tract. While primary carcinoma may develop anywhere along the course of the duodenal sweep, the region of the ampulla of Vater is the most common site (b/c the gall bladder empties there also), and the duodenal bulb the least common site. IV. - SMALL BOWEL The small bowel may be associated with malabsorption syndromes, parasitic infestations, enteric infections, and may be affected by neoplasms (benign and malignant), metastatic and primary. A number of disorders are associated with the radiologic "malabsorption" pattern. The most common are sprue "gluten-induced enteropathy" and lymphoma. Less frequent causes include radiation enteritis, Whipple's disease, eosinophilic syndrome with small bowel involvement, eosinophilic gastroenteritis, ischemia, mastocytosis, and pancreatic exocrine deficiency. Barium studies classically show moderate dilatation of the entire small bowel (2-4 cm norm). The valvulae conniventes (2-4 mm norm) are generally prominent. And there may be reversal of the normal ratio of jejunal and ileal folds -- the so-called "flip-flop" pattern -- characteristic of sprue, as can be seen on this slide (you should have jejunal > ileal folds). The number of folds per inch is decreased in the jejunum and increased in the ileum, i.e., the reverse of the normal small bowel fold count. Unfortunately, the abnormal findings of the small bowel are very non-specific. (Slide #19) A small bowel series in this 64-year-old woman reveals prominence of the valvulae conniventes in a dilated small bowel. She had presented with steatorrhea, weight loss, and arthritis. The scattered 2 - 3 millimeter filling defects in the proximal jejunum represent mucosal nodules characteristic of this disease. In this day of AIDS, cryptosporidiosis should not be forgotten. (Slide #20) This 31-year-old intravenous drug abuser complained of relentless diarrhea and severe weight loss. A small bowel series showed dilution of the barium by excessive secretions. There is marked thickening of the mucosal folds of the duodenum and the valvulae conniventes of the small bowel due to edema. Note the tubular characterless appearance of the distal small bowel. No discussion of the small bowel can be complete without mentioning Crohn's disease (aka terminal ileaitis). Crohn's disease may involve any portion of the digestive tract including the oral pharynx, esophagus, and stomach. Can occur mouth to anus; anywhere in the GI tract; any part or all of the GI tract. Skeletal manifestations are not uncommon. Crohn's colitis is pictured here with this skip lesion. (Slide #21) This is the barium enema performed on a 26-year-old woman with diarrhea and weight loss. It shows segmental narrowing of the descending colon and proximal sigmoid colon. The mucosa is markedly irregular and nodular. Note the aphthous ulcerations and pseudo polyps on the detail view. The slide on your right reveals a second area of involvement in the mid transverse colon. Here manifestations include narrowing, loss of haustrations in a granular mucosa. The remainder of the colon looks normal including the rectum. (Slide #22) This is typical ileocecal involvement in Crohn's disease. This 45-year-old woman had a long history of "mucosy" diarrhea and weight loss. A spot film of a small bowel series shows a fixed "C" loop GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 5 of 6 of the terminal ileum with sacculations, narrowing, and several tight strictures. The configuration of the infected loop indicates the presence of an inflammatory mass in the adjacent mesentery. The cecum has a conical configuration due to entrance involvement by Crohn's disease. Note the mass effect on the cecum and the terminal ileum caused by an inflammatory mass in the adjacent mesentery. Finally as our population has aged and lived longer, and as the young adult population has found more and more things to inject into their bodies, small bowel ischemia has increasingly become a topic for discussion. (Slide #23) The slide shown above is of a 25-year-old woman with long-standing lupus erythematosus who presented to the Emergency Room with severe and acute abdominal pain. The barium enema with reflux into the terminal ileum shows marked thumb-printing and a "stacked-coin" appearance with separation of adjacent loops. A CT of the pelvis (middle figure) shows a narrowed loop of ileum marked with thickening of its wall (arrow 1). The normal uterus is seen below the ileum (arrow 2). The CT scan on your right is a higher cut showing the thickening of the small bowel mesentery. Small bowel ischemia is most commonly associated with congestive heart failure, cardiogenic shock, lupus erythematosus, mesenteric venous thrombosis, and atherosclerosis of both small and large vessels. Associated radiographic findings may be pneumatosis intestinalis and or portal venous air. V. - COLON Although other imaging modalities such as ultrasound, computed tomography, magnetic resonance, and angiography are used to evaluate the colon, the barium enema remains the basic method of radiologic assessment. Whether to employ the single or double contrast technique has been the subject of spirited debate over the past two decades. Double-contrast barium enema is preferred by sub-specialists and has become the more frequent type of colon examination at most hospitals Colonoscopy complements radiographic examination of the colon and may resolve questions unanswered by the latter. Colonoscopy has important limitations: It sometimes fails to evaluate the right colon; it does not give a general overview of the colon; it generally does not provide permanent visual record; and it is substantially more expensive (in the United States) then either the single-contrast or double-contrast enema. Diverticulosis and diverticulitis are frequent findings on barium enema of the colon. (Slide #25) Here a perforated sigmoid diverticulum is observed in a 65-year-old man presented with lower abdominal pain of acute onset with this and had associated fever and vomiting. Barium enema shows scattered sigmoid diverticulum with free spill of barium into the peritoneal cavity. The leakage of barium from the apex of the large diverticulum is seen in the slide on your right. Appendiceal abscess with an appendicoliths: (Slide #26) This teenage girl with spina bifida and ventriculoperitoneal shunt had right lower quadrant pain and fever for several days. Physical examination revealed a tender right lower quadrant mass. The more superior image A reveals a fold soft tissue mass measuring approximately 8 centimeters by 6 centimeters in the right lower quadrant of the abdomen. Within this region two oval laminated calcifications typical of appendicoliths may be observed. On the two CT images, B and C, the more superior is obtained at the level of the ascending colon and reveals a gas containing soft tissue mass displacing the cecum (arrow 1) medially. A loop of ileum (arrow 2) is draped over the mass. On a more caudal cut, the more inferior CT examination, the appendicoliths are seen within the mass, which lies lateral to the cecum (arrow). The appendix itself cannot be identified. A positive CT Scan rules in an appendicitis, but a negative CT Scan does not rule it out. A positive CT confirms it only if you have: a symptomatic pt., rocks in the appendix, and an inflammatory mass in the appendiceal area. Ulcerative colitis is a proctocolitis that extends approximately to a variable extent; in its severest form, the entire colon is affected. The incidence is in the third and fourth decades; however, the disease may appear as late as the sixth decade. GI 2 #6 Tue Feb. 24, 2004, 10-11 a.m. Dr. Pat G. Sharratt, D.O. Malik Ali Page 6 of 6 The earliest radiologic manifestation of ulcerative colitis is the granularity of the rectal and colic mucosa, which may be best seen on a double-contrast barium enema examination. This is an acute ulcerative colitis on the left and progression on the right. This 14-year-old boy had several month history of bloody diarrhea. Barium enema on the left shows pan-colitis with extensive ulceration of the sigmoid colon. The ulcers are symmetrical and of the collar-button type. The slide on the right shows 5 years later. A double-contrast barium enema shows a narrowed ahaustral sigmoid and descending colon. The affected segments have a granular mucosa. Ulceration is no longer evident. There are a tremendous number of infectious colitis etiologies. In my opinion, one of the most important is atrogenically induced infectious colitis caused by clostridium diphicele. It is almost always secondary to antibiotic therapy with lincomycin being the primary offender. This is a 29-year-old man who developed explosive non-bloody diarrhea several days after undergoing transplantation. On this barium enema, note the extensive edema of the entire colon with the prominent mucosal ridges. Although the mucosal contour is shaggy and irregular, there is no evidence of ulceration. The descending and transverse colon are spastic and ahaustral. Sigmoidoscopy revealed extensive pseudomembrane formation. The patient’s condition improved dramatically after cessation of antibiotic therapy (iatrogenically induced). Not so new but interesting things are seen more frequently on barium enema examination, and I include these only as aside in view of the prevalence of sexually transmitted diseases including AIDS. This first slide is condolyma acuminata with associated carcinoma of the rectum. This is a 40-year-old homosexual man who has the typical verrucus warts on the perineum and a bloody rectal discharge. Barium enema showed a smooth dome-like mass arising at the anal verge and extending intraluminally. Also note the irregular crescentic deformity of the rectal wall (arrows). At proctoscopy, the latter proved to be an ulcerating carcinoma. Although malignant degeneration of condyloma is a recognized complication, the two lesions were unrelated in this patient. Gonococcal proctitis: This 28-year-old homosexual man complained of tenesmus and rectal discharge. Frontal and lateral views of barium enema show severe spasm and ulceration of the rectum. Gonococcus was cultured from rectal secretions. This is an example of malignant degeneration in an edematous polyp. This 70-year-old man presented with rectal bleeding. On the left single and on the right, double-contrast films from a barium enema show multilobular sessile mass in the sigmoid colon. The lesion measures 3 x 2 x 2 centimeters. Note the 1centimeter area of puckering at its attachment to the bowel wall, a finding that strongly suggests neoplastic invasion. Endoscopy revealed an adenocarcinoma arising in an adenomatous polyp. Ischemia of the colon is usually secondary to atherosclerosis of the mesentery circulation (small or large vessels); less often it is The large bowel is also subject to ischemia. due to vasculitis such as lupus erythematosus, a low flow state following surgery, hemorrhagic shock, veno-occlusive disease, venous thrombosis or rarely Burger's. Patient typically presents with acute abdominal pain and diarrhea, passing mucus and small amounts of blood by the rectum. Some persons have little or no pain. This is a 32-year-old woman who developed acute abdominal pain and bloody diarrhea while receiving chemotherapy for choriocarcinoma. A barium enema shows extensive thumbprinting of the transverse colon and proximal descending colon. There is marked spasm of the involved bowel segments. These changes which are most likely secondary to mesentery venous thrombosis resolved completely after several days. Blood supply to colon: superior and inferior mesenteric arteries. Superior gives rise to the right and middle colic arteries whereas the inferior gives rise to the left colic artery.