file - BioMed Central
advertisement

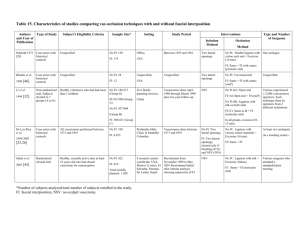
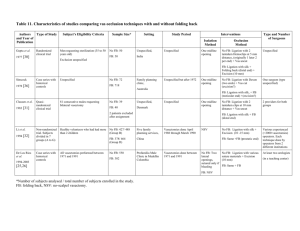
Table 23. Characteristics of studies comparing vas occlusion techniques with and without leaving the testicular end open Authors Type of Study and Year of Publication Shapiro and Silber Prospective cohort study Subject’s Eligibility Criteria Sample Size* Setting Study Period Interventions Isolation Method Unspecified. Close-ended only from St-Louis, Missouri 1979 [15] O: 433 Unspecified, 410 from Canada Canada 23 from Missouri USA 1 year (78?) Unspecified 1983 [48] Case series with historical controls Unspecified O: 4 C: 387 Method O: Ligation with Hemoclip (n=?) (262) or TC (Concept®) on prostatic end (148 + 23) Two urologists C: TC on both ends. C: 91 Goldstein Occlusion Type and Number of Surgeons Excision in both groups? Out-Patient clinic in Unspecified tertiary care university hospital, Two lateral incisions O: Excision (5 mm) + TC (5 mm) on prostatic end One urologist C: ? USA Errey and Edwards 1986 [13] Moss 1992 [14] Li et al. 1994 [32] Case series with historical controls Unspecified Case series with historical controls Unspecified Non-randomized trial. Subjects divided in 7 groups (A to G) Healthy volunteers who had had more than 2 children O: 4,330 Out Patient Fertility O: 1979 to June 1984 Control Clinic, C: 1976 to 1979 Australia Two lateral incisions O: 3,139 (3,103?) Unspecified, C: 3,081 USA O: October 1979 to April 1992 One midline opening O: Same as close-ended but testicular end uncauterized C: June 1972 to September 1979 Until 1989 and NSV thereafter C: TC on both ends +FI on prostatic end with an Hemoclip. Vasectomies performed from April 1988 to March 1990 + a 2-year follow-up period NSV O: Ligation with silk on prostatic end and FI (200) or not (215) C: 3,867 O: 369/415 (group A and G) Five family planning services, C: 2,004/2,298 (group B, C, D, E, and F) China O: Same as close-ended but testicular end uncauterized One provider C: Ligation with Nylon 3-0 + Excision (2-5 mm) + EC on both ends + FI on prostatic end + FB of both ends. C: Various occlusive methods but all close-end One gynaecologist Various experienced (>2,000 vasectomies) operators. Each technique done by operators from 2 different institutions Excision(10 -15 mm) in all groups excepted D Labrecque et Case series with al. 1998 [33] concurrent controls All men with a first bilateral vasectomy between 1994 and 1996 O: 322/448 C: 545/775 Excluded: technique not performed as usual (n=9) O: Family planning clinic in a tertiary care hospital January 1994 to February 1996 NSV C: Office, C: Ligation with 2 Hemoclips per vas + Excision (10 mm) Canada Labrecque et al. 2002 controls [34] Case series with concurrent controls All men with a first bilateral vasectomy between 1996 and 2000 Excluded: vas impossible to expose due to technical difficulties (n =7, 0.2%) O: 1,165 / 1,721 C: 1,453 / 2,040 O: Family planning clinic in a tertiary care hospital (n=1086) and office (n=635) C: Office O: TC (10 mm) + one Hemoclip on prostatic end + FI on open testicular end + Excision (10 mm) O: July 1996 to November 2000 (n=1,086) October 1999 to November 2000 (n=635) C: July 1996 to October 1999 NSV O: TC (10 mm) + FI on prostatic end + Open testicular end + Excision (10 mm) (n=151), otherwise no excision C: Ligation with 2 Hemoclips per vas + Excision (10 mm) *Number of subjects analysed / total number of subjects enrolled in the study. O: Open-ended, C: Close-ended, TC: thermal cautery, EC: electro-cautery, FI: fascial interposition, FB: folding back, NSV: no-scalpel vasectomy. All performed by or under the supervision of (1/3 of hospital cases) one general practitioner One general practitioner Table 24. Outcome measures of studies comparing vas occlusion techniques with and without leaving the testicular end open Authors and Year of Publication Shapiro and Silber Effectiveness Data Collection Timing of SA 1994 [32] Method of Follow-up Main Outcome Measures No number, motility, nor time specified Prospective Unspecified Examination at 1 week and then at monthly intervals Granuloma, pain , epididymitis Retrospective 15 ejaculations post vasectomy After 15 ejaculations. If motile sperm, repeat SA 2 weeks later and at 3 and 5 months. Motile sperm after 5 months. No number specified N/A N/A N/A Complications unspecified in the closeended group Retrospective 1 year Unspecified No number, motility, nor time specified Retrospective 1 year Spontaneous medical consultations Granuloma: Nodule or cyst at the point of interruption of the vas after the immediate postoperative tenderness had subsided, painful to pressure or during ejaculation; Epididymitis: Tender swelling of all or part of the epididymis tender lumps in it, whether solid or cystic, or complaints of orchialgia in the absence of any detectable abnormality; cutaneous fistula Retrospective Unspecified but variable 2, 4 and 12 months postoperatively No number, motility, nor time specified Retrospective Unspecified Spontaneous medical consultations Epididymitis: Pain and tenderness of the testicle on one side. Follow-up visits every six months Bleeding, infection, stasis 1992 [14] Li et al. Definition of Failure Length of Follow-up After 15 ejaculations then monthly even after azoospermia 1986 [13] Moss Data Collection Unspecified but variable 1983 [48] Errey and Edwards Post-vasectomy Semen Analysis (SA) Prospective 1979 [15] Goldstein Length of Follow-up Complications Prospective 2 years 6 months intervals until 2 years post vasectomy Presence of sperm two years Prospective after vasectomy 2 years Hematomas: mass in the scrotum Table 24. Outcome measures of studies comparing vas occlusion techniques with and without leaving the testicular end open (continued) Authors and Year of Publication Labrecque et al. Effectiveness Data Collection Retrospective 1998 [33] Length of Follow-up At least 4 months but variable Complications Post-vasectomy Semen Analysis (SA) Timing of SA 3 months Data Collection Definition of Failure Early recanalization: motile sperm after 3 SA or 6 months, or second SA with increasing number of motile sperm Length of Follow-up Method of Follow-up Retrospective At least 4 months but variable Spontaneous medical consultations Granuloma (painful lump at the surgical site), vasi-orchi-epididymitis (swelling and pain without infection signs), hematomas (lump at the surgical site within few hours after surgery), infection (any prescription of antibiotics), pain (no diagnostic otherwise), non infectious painful syndrome (granuloma, vasi-orchiepididymitis and pain combined) Retrospective At least 4 months but variable Spontaneous medical consultations Surgical (hematomas with or without infection, and infection - defined as any antibiotics prescribed), non-infectious pain (painful granuloma, vasitis/orchiepididymitis, and pain with no specific diagnosis), other (such as hemospermia, sexual dysfunction, pain localized at the wound, isolated scrotal ecchymosis) Late recanalization: pregnancy and reappearance of motile sperm Labrecque et al. 2002 controls Retrospective At least 4 months but variable [34] SA: semen analysis, N/A: not applicable. 2 to 3 months then every 6 weeks until success or failure Possible failure: Last SA showing any motile sperm or last 2 SA with 1x109/L non-motile sperm, and last SA done >91 days postvasectomy, and not classified as confirmed failure. Confirmed failure: 3 SA showing any motile sperm, or 2 SA with 1x109/L sperm with any motility, and last SA done >91 days post-vasectomy; or last SA done >182 days post-vasectomy showing 1x109/L sperm with any motility. Main Outcome Measures No ? Yes Yes No ? No No Yes Goldstein 1983 [48] 3 391 0.06 ? No ? Yes ? No ? No Yes ? ? ? No ? Errey and Edwards 3 8197 1.0 ? No Yes Yes Yes Yes ? Yes No ? ? ? No ? Yes No No 3 6220 1.0/ ? No ? Yes No Yes ? No No ? Yes Yes No ? Yes No No Yes No No Yes No Yes No Yes ? Yes Yes Yes O: 89% No No Yes Global Assessment No Follow-up Rate* Systematically Performed in All Men ? Adequate Assessment* Blinded No At the Same Time Explicit Criteria Yes Adequate Assessment* No Sample Size No Follow-up Yes Provider ? Setting 0.33 Study Period 524 Participants 2 Shapiro and Silber Power* Systematically Performed in All Men Follow-up Rate* Complication Assessment Blinded At the Same Time Effectiveness Assessment Compliance/ Follow-up rate Adequate Comparability* Explicit Criteria Comparability Total Sample Size Study Design* Authors and Year of Publication Table 25. Quality assessment of studies comparing vas occlusion techniques with and without leaving the testicular end open No ? Low N/A N/A Very Low No No ? Low No No No ? Very Low Yes Yes No O: 89% Moderate 1979 [15] 1986 [13] Moss 0.58† 1992 [14] Li et al. 2 2373 0.87 C: 87% 1994 [32] Labrecque et al. 3 1223 0.71 Yes No No Yes No ± Yes No Yes ? Yes Yes Yes O: 70% C: 87% Yes No No No No ? Low No No No No No ? Moderate C: 72% 1998 [33] Labrecque et al. 3 3761 0.99 Yes No No Yes ± Yes Yes 2002 controls [34] *Criterion used for global assessment (see Table 2, Additional file 1). † power for failure, infection, and hematomas / congestive epidydimitis. O: Open-ended, C: Close-ended, N/A: not applicable. Yes Yes Yes Yes Yes Yes O: 68% C: 71% Table 26. Results of studies comparing vas occlusion techniques with and without leaving the testicular end open Authors and Year of publication Shapiro and Silber Effectiveness (Failure) Based on SA O: 9 (2.1%) Based on Pregnancy Unspecified C: 0 1979 [15] Goldstein O: 2 (50%) 1983 [48] C: 1 (0.3%) O: 1 (0.02%) Infections Higher failure risk with open than with closeended, most with cautery (7/9) Unspecified Significantly higher failure risk with open than with close-ended. Very small sample size Unspecified Similar failure risk P < 0.00005 Errey and Edwards Comments Complications Hematoma C: 3 (0.08%) O: 1 (0.03%) O: 0 (0%) 1992 [14] C: 0 (0%) C: 1 (0.03%) Similar failure risk Granuloma Epididymitis O: 0 O: 420 (97%) O:0 C: 1 (1%) C:4 (4%) C: 1 (1%) Others Total Only one patient, with close-ended, had pain associated with epididymitis O: 66 (1.5%) O: 64 (1.5%) Fistula C: 122 (3.2%) C: 106 (2.7%) O: 1 (0.02%) P < 0.001 P < 0.001 C: 1 (0.03%) O: 2 (0.06%) O: 2 (0.06%) O: 6 (2%) C: 0 (0%) C: 1 (0.03%) C: 18 (6%) Significantly lower risk of epididymal congestion and painful granuloma with openended Similar risk of complications but significantly lower risk of epididymitis with openended N=300 in O and C; p < 0.05 Li et al. O: 15 (4.1%) O: 2 ( 0.5%) 1994 [32] C: 63 (3.1%) C: 25 (1.2%) Labrecque et al. O: 3 (0.9%) O: 1 (0.3%) 1998 [33] C: 13 (2.4%) C: 2 (0.4%) Labrecque et al. 2002 controls O: 3 (0.3%) [34] C: 126 (8.7%) Bleeding: Similar failure risk but almost all failures (14/15) O: 7 (1.9%) with O were without FI C: 5 (0.2%) O: 1 (0.3%) O: 0 (0%) C: 6 (0.3%) C: 2 (0.1%) O:14(3.1%) Painful C 9 (1.2%) granulomas Vasi-orchiepididymitis O: 6 (1.3%) O: 18 (4.0%) C 6 (0.8%) C: 15 (1.9%) Similar risk of infection and stasis but higher risk of complications with open-ended (all without FI). Total risk of (undefined) complications very low Non significant (P = 0.14) lower failure (early + late) risk with open-ended. O: 5 (1.1%) O: 12 (2.7%) C: 4 (0.5%) C: 5 (0.6%) Significant lower failure risk with open-ended O: 5 (0.2%) O: 2 (0.1%) O:12(0.7%) O: 14 (0.8%) O: 47 (2.7%) Surgical: C: 26 (1.5%) C: 5 (0.2%) C:11(0.5%) C: 20 (1.0%) C: 43 (2.1%) O: 28 (1.6%) P < 0.0001 O: 55 (12.3%) Higher risk of painful granulomas, vasi-orchiC: 39 (5%) epididymitis, and pain P < 0.0001 with open-ended C: 10 (0.5%) P = 0.0005 Non infectious pain O: 71 (4.1%) C: 72 (3.5%) P = 0.34 SA: semen analysis, O: open-ended, C: close-ended. Comments Complications with close-ended unspecified 1986 [13] Moss Pain Similar risk of non infectious postvasectomy pain but higher risk of surgical complications (hematomas) with openended