FI: fascial interposition, NSV
advertisement

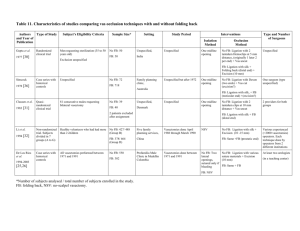
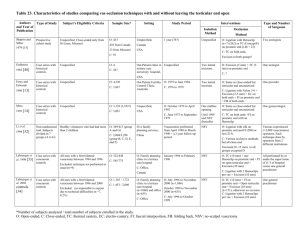
Table 15. Characteristics of studies comparing vas occlusion techniques with and without fascial interposition Authors Type of Study and Year of Publication Schmidt 1973 [20] Case series with historical controls Subject’s Eligibility Criteria Sample Size* Setting Study Period Interventions Isolation Method Unspecified No FI: 150 Office, FI: 135 USA Between 1955 and 1961 Two lateral openings Occlusion Type and Number of Surgeons Method No FI: Double ligation with One urologist cotton each end + Excision (10 mm) FI: Same + FI with suture (prostatic end) Rhodes et al. 1980 [46] Li et al. 1994 [32] Case series with historical controls Unspecified Non-randomized trial. Subjects divided in 7 groups (A to G) Healthy volunteers who had had more than 2 children No FI: 28 Unspecified, FI: 12 USA No FI: 186/215 (Group G) Five family planning services, FI:183/200 (Group A) China Unspecified Vasectomies done April 1988 through March 1990 plus two-year follow-up Two lateral openings No FI: Vas transected NSV No FI (G): Open-end 1994-2003 Case series with historical controls All vasectomies performed between 1971 and 1991 (Group B) FI: 380/431 (Group C) In all groups, excision (1015 mm) No FI: 550 FI: 4,015 Profamilia Male Clinic in Medellin Colombia Vasectomies done between 1971 and 1991 2003 [45] Randomized clinical trial Healthy, sexually active men at least 18 years old who had chosen vasectomy for contraception No FI: 422 FI: 419 Total initially planned: 1,200 *Number of subjects analysed/total number of subjects enrolled in the study. FI: fascial interposition, NSV: no-scalpel vasectomy. 8 research centers worldwide: USA, Mexico (2 sites), El Salvador, Panama, Sri Lanka, Nepal No FI: Two lateral openings FI: Two lateral openings, sutured only if bleeding (41%) and NSV (59%) [25,26] Sokal et al. FI: Same + FI with suture (end?) Various experienced (>2,000 vasectomies) FI (A) Open-end + FI (end?) operators. Each technique done by No FI (B): Ligation with operators from 2 silk on both ends different institutions FI (C): Same as B + FI (testicular end) No FI: 427/488 De Los Rios et al. Unspecified Recruitment from November 1999 to May 2001 Recruitment halted after interim analyses showing superiority of FI NSV No FI: Ligation with various suture materials + Excision (10 mm) At least two urologists (in a teaching center) FI: Same + FI No FI : Ligation with silk + Excision (10mm) FI : Same + FI (testicular end) Various surgeons who attended a standardization meeting Table 16. Outcome measures of studies comparing vas occlusion techniques with and without fascial interposition Authors and Year of Publication Schmidt Effectiveness Data Collection Method of Follow-up Main Outcome Measures No number, motility nor Retrospective time specified. Sterility with 2 negative specimens, 1 month apart Unspecified but variable Unspecified Granuloma: leakage of sperm from the proximal vas Retrospective Unspecified but variable Unspecified No number, motility nor time specified but SA results in failure described N/A N/A N/A Prospective 2 years 6 months intervals until 2 years post vasectomy Presence of sperm two years Prospective after vasectomy 2 years Follow-up visits every 6 months Bleeding, infection, stasis Retrospective At least 3 months but variable 3 months or after 20 ejaculations Presence of live spermatozoa four months after vasectomy Unspecified Early postvasectomy follow-up visit and spontaneous medical consultations Infection, bleeding, pain, granuloma, orchi-epididymitis, sexual dysfunction Prospective 12 months 2 weeks, then every 4 weeks Early: > 5 million motile Prospective through 34 weeks or until sperm/mL at 14 weeks or success or failure, and 52 later weeks Late: motile sperm at > 26 weeks or later (>10% motile and >100,000 sperm/mL) 12 months Follow-up visits at the time of SA Surgical difficulties and adverse events: pain, sperm granuloma, orchiepididymitis, hematoma, infection 1994-2003 [25,26] Sokal et al. Definition of Failure Length of Follow-up Unspecified 1994 [32] De Los Rios et al. Timing of SA Data Collection Unspecified but variable 1980 [46] Li et al. Post-vasectomy Semen Analysis (SA) Retrospective 1973 [20] Rhodes et al. Length of Follow-up Complications 2003 [45] N/A: not applicable, SA: semen analysis. N/A Retrospective No No ? Yes ? No ? Rhodes et al. 1980 3 40 0.08 ? No ? ? No ± Yes No No ? Yes ? No 97.5% 2 807/ 369† 0.70/ No Yes No No Yes Yes Yes Yes Yes ? Yes Yes Yes 88%/89%† No No Yes ? Global Assessment ? Adequate Assessment* Yes Sample Size No Follow-up Yes Provider ? Setting No Study Period ? Participants 0.32 Power* 285 Follow-up Rate* Systematically Performed in All Men ? 3 Adequate Assessment* Blinded No Schmidt 1973 [20] At the Same Time Explicit Criteria No Systematically Performed in All Men Follow-up Rate* Complication Assessment Blinded At the Same Time Effectiveness Assessment Compliance/ Follow-up rate Adequate Comparability* Explicit Criteria Comparability Total Sample Size Study Design* Authors and Year of Publication Table 17. Quality assessment of studies comparing vas occlusion techniques with and without fascial interposition No ? Very Low N/A N/A Very Low Yes No 88%/89%† Moderate [46] Li et al. 1994 [32] De Los Rios et al. 0.39† 3 4565 0.97 Yes No Yes No Yes No ? No Yes No Yes ? No 55% No No Yes ? No 55% Very Low 1 841 0.86‡ Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No FI: 98.6% No No Yes Yes No 6 weeks High 1994-2003 [25,26] Sokal et al. 2003 [45] FI: 97.9% 100% 12 months 89% *Criterion used for global assessment (see Table 2, Additional file 1). FI: fascial interposition, N/A: not applicable. † group A and G / group B and C. ‡ Sample size when study halted (n=841)/sample size initially planned (n=1,200). Table 18. Results of studies comparing vas occlusion techniques with and without fascial interposition Authors and Year of publication Effectiveness (Failure) Based on SA Schmidt No FI: 3.3% 1973 [20] FI: 0% Rhodes et al. No FI: 6 (21.4%) 1980 [46] Based on Pregnancy Comments Complications Hematoma Infections Pain Lower failure risk with FI when ligation /excision performed Granuloma Epididymitis Others Total No FI: 6.0% No other complication specified. Higher risk of granulomas defined as sperm leakage with FI FI: 9.7% Similar failure risk with and without FI when only vas transected. Very small sample size FI: 2 (16.7%) Comments Complications unspecified P = 0.55 Li et al. 1994 [32] No FI (G): 14 (7.5%) No FI (G): 1 (0.5%) FI (A) :1 (0.6%) FI (A) :1 (0.6%) No FI (B): 6 (1.4%) FI (C):10 (2.6%) No FI (B): 2 (0.5%) B vs C: Higher failure risk with FI (testicular) when ligation/excision is performed FI (C): 6 (1.6%) Large variation between centers De Los Rios et al. No FI: 94 (29.1%) 1994-2003 FI: 57 (2.6%) [25,26] Sokal et al. 2003 [45] G vs A: Lower failure risk with FI when openend is performed Bleeding No FI (G): 7 FI (A) :0 No FI (B):0 No FI (G): 1 FI (A): 0 Stasis No FI (B): 2 No FI (G): 0 FI (A) :0 FI (C): 1 No FI (B):0 FI (C): 0 FI (C): 1 No FI (G): 8 (2.2%) FI (A): 0 No FI (B): 2 (0.5%) FI (C): 2 (0.5%) 0 Lower failure risk with FI when ligation /excision performed No FI: 53 (12.7%) No FI: 2 (0.5%) FI: 24 (5.9%) FI: 2 (0.5%) P < 0.0008 SA: semen analysis, FI: fascial interposition. Lower failure risk with FI when ligation /excision performed Time to azoospermia and to severe oligospermia shorter with FI (P < 0.0001) Higher risk of complications due to bleeding in group G (open-end without FI). Total risk of (undefined) complications very low Complications unspecified No FI: 6 (1.4%) No FI: 2 (0.5%) FI: 6 (1.4%) FI: 2 (0.5%) 52 weeks No FI: 14 (4.3%) FI: 9 (2.6%) No FI: 29 (6.9%) No FI: 6 (1.4%) FI: 41 (9.8%) FI: 12 (2.9%) 6 weeks No FI: 62 (14.7%) FI: 74 (17.7%) P = 0.23 Non significant higher risk of complications due to granuloma and orchiepididymitis with FI. Same risk of hematoma and infection