Pediatric Emergencies - Emergency Medical Responder
advertisement

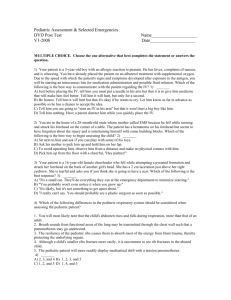
Ready for Review Sudden illnesses and medical emergencies are common in children and infants. Because the anatomy of children and infants differs from that of adults, special knowledge and skills are needed to assess and treat pediatric patients. Managing a pediatric emergency can be a stressful situation for emergency medical responders. Because both the child and the parents may be frightened and anxious, you must behave in a calm, controlled, and professional manner. A child’s airway is smaller in relation to the rest of the body; therefore, secretions and swelling from illnesses or trauma can more easily block the child’s airway. Because the tongue is relatively larger than the tongue of an adult, a child’s tongue can more easily block the airway. Hyperextension of a child’s neck can occlude the airway. The child who is unresponsive, lackluster, and appears ill should be evaluated carefully because the lack of activity and interest signal serious illness or injury. After you conduct your primary assessment, you should carry out the routine patient examination, paying special attention to mental awareness, activity level, respirations, pulse rate, body temperature, and color of the skin. The pediatric assessment triangle is designed to give you a quick general impression of the child using only your senses of sight and hearing. The three components of the pediatric assessment triangle are overall appearance, work of breathing, and circulation to the skin. It is important for you to open and maintain the patient’s airway and to ventilate adequately any child with respiratory problems. Otherwise, the child may experience respiratory arrest, followed by cardiac arrest. Cardiopulmonary resuscitation for children and infants differs from adult cardiopulmonary resuscitation in several important ways. You should be certain that you understand these differences and are able to perform the appropriate steps confidently in the field. Suctioning removes foreign substances that you cannot remove with your gloved fingers from the airway of a child. Oral airways can be used to maintain an open airway after you have opened the child’s airway by manual means. Young children often obstruct their upper and lower airway with foreign objects, such as small toys or candy. If the object is only partially blocking the airway, the child should be able to pass some air around it. You should attempt to remove the object only if it is clearly visible and you can remove it easily. In complete or severe airway obstruction in a conscious child, you should perform the Heimlich maneuver (abdominal thrusts). If the child becomes unresponsive, you should begin cardiopulmonary resuscitation. To relieve an airway obstruction in an infant, use a combination of back slaps and chest thrusts. Children in respiratory distress require immediate medical attention. Signs of respiratory distress include a rapid or slow breathing rate, nasal flaring, retraction of the skin between the ribs and around the neck muscles, stridor, cyanosis, altered mental status, and combativeness. Respiratory distress can lead to respiratory failure, which in turn can lead to circulatory failure. Three serious respiratory problems in pediatric patients are asthma, croup, and epiglottitis. A child who has asthma is usually already being treated for the condition by a physician; your primary treatment consists of calming and reassuring the parents and the child. Croup is an upper airway infection that results in a barking cough. Although epiglottitis resembles croup, it is a serious respiratory emergency and you must arrange for prompt transport. Other pediatric medical emergencies include drowning, heat-related illnesses such as heatstroke, high fevers, seizures, vomiting and diarrhea, and abdominal pain. Children’s natural curiosity may lead them to sample medications or household items that contain poisonous substances. The two most common types of poisonings in children are caused by ingestion (taken by mouth) and absorption (entering through the skin). Sudden infant death syndrome, also called crib death, is the unexpected death of an apparently healthy infant. You should know your local guidelines for the management of sudden infant death syndrome. Remember that the parents could do nothing to prevent the death. When caring for pediatric trauma patients, remember that you may have to adapt materials and equipment to the child’s size. Also remember that children do not show signs of shock as early as adults, although they can progress into severe shock quickly. Major trauma in children usually results in multiple system injuries. Your first priority is always to check the ABCs and then stop severe bleeding, treat for shock, and proceed with the physical examination. If you suspect child abuse or sexual assault, you must transport the child to an appropriate medical facility.