The deteriorating child * what is our vector, Victor?
advertisement
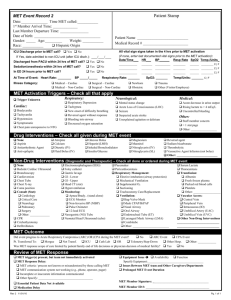
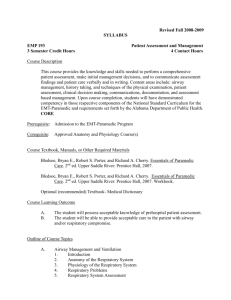
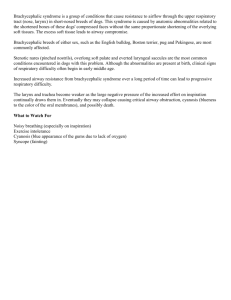
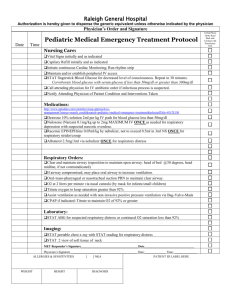
The Deteriorating Child – what is our vector, Victor? Adam Skinner Staff Anaesthetist Royal Children’s Hospital 30th July 2015 Aims Review anatomical and physiological differences between adults and children and link with clinical features seen in children in recovery. Discuss the (my) thought process when managing acute hypoxia and bradycardia in a child. Discuss ViCTOR and its current practical role in recovery. Children vs Adults Airway differences Oxygen balance differences Cardiac differences Children vs Adults Airway differences Oxygen balance differences Cardiac differences The ‘Normal’ Airway Adult Infant Holding an Airway Airway Oedema Laryngospasm Children vs Adults Airway differences Oxygen balance differences Cardiac differences Demand vs Supply Oxygen Consumption Demand vs Supply Oxygen Uptake Respiratory Drive Rib Cage and diaphragm mechanics Volumes and Elastic forces Oxygen Uptake Respiratory Drive Rib Cage and diaphragm Mechanics Volumes and Elastic forces Oxygen uptake – Respiratory drive Immature Respiratory Centre (Neonates) Opioid Sensitivity Neonates Genetics Co-morbidity (eg CP, OSA) Opioid sensitivity - codeine Codeine Variability Oxygen Uptake Respiratory Drive Rib Cage and diaphragm Mechanics Volumes and Elastic forces Chest Mechanics Chest wall differences Infant Adult Oxygen Uptake Respiratory Drive Rib Cage and diaphragm Mechanics Volumes and Elastic forces Elastic Forces Cardiac Differences Bradycardia– GIVE OXYGEN!! Scenario 1: 5 year old 23 kg in recovery for tonsillectomy for obstructive sleep apnoea. Rapid desaturation to 60%, cyanosed Initial Action Buzzer Mask, T-Piece 100% OXYGEN Position Patient and airway Inflate lungs Scenario 1 Can’t inflate lungs Why? What do we need? Who do we need? Laryngospasm Scenario 2: 5 year old 23 kg in recovery for tonsillectomy for obstructive sleep apnoea. Saturation 78%, shallow breathing. Initial Action Buzzer Mask, T-Piece 100% OXYGEN Position Patient and airway Inflate lungs Scenario 2 Able to inflate with temporary improvement in saturations What is going on? Maybe difficult to diagnose in children Scenario 3 5 year old 23 kg in recovery for tonsillectomy for obstructive sleep apnoea. Noted on monitor to be bradycardic at 60 beats per minute. How do we assess and manage? Initial Action Buzzer Mask, T-Piece 100% OXYGEN Position Patient and airway Inflate lungs Are we starting CPR? What is normal? Arch Dis Child. August 2015 Normal Values What is ViCTOR? What is ViCTOR? National Standard 9: Recognition and response of the deteriorating patient Key element - recording of patient observations - greater emphasis on ‘Human Factor’ principles in the design of charts Paediatric Clinical Network Initiative Examples of Track and Trigger Charts 1 – 4 year old Observation and Response Chart: Service Normal Range (white area) RESPIRATORY RATE MET or CODE trigger point Clinical review trigger point (high) RCH *trial chart 20 – 40 41 High 56 / Low 16 Eastern Health 21 – 30 31 High 36 / Low 11 Barwon Health 20 – 40 41 Highest 60 / Lowest 15 * 3 tier escalation Bendigo Health 21 - 35 36 Highest 41 / Low 14 The Alfred 21 – 49 50 High 60 / Low 15 Austin Health 20 – 40 41 Highest 60 / Lowest 20 * 3 tier escalation NSW 20 – 40 41 Highest 60 / Lowest 15 * 3 tier escalation SA 20 – 34 35 Highest 40 / Lowest 12 * 3 tier escalation 5 age groups • 0 - 3 months • 3 - 12 months • 1 - 4 years • 5 - 11 years • 12 - 18 years Paediatric Clinical Network Initiative Percentile curves for HR and RR in hospitalized children Bonafide C P et al. Pediatrics 2013;131:e1150-e1157 ©2013 by American Academy of Pediatrics What is the point of ViCTOR for recovery? What is the point of ViCTOR for recovery? “Tool for communication and justification” Sharon Kinney PhD, RCH. Forces the team to consider the patient with objective measurements (IN CONTEXT) outside ‘normal’ EARLY. Provides communication framework between specialities, wards and hospitals. Mandates response in a timeframe with suggested roles. At the moment we use it in PACU just before transfer. Summary Physiology link with Clinical Interpretation By recognising human factors we can better recognise and managing critical incidents in recovery as a team. PRACTICE with multi-disciplinary scenarios if possible!