Gastrointestinal Vivas
advertisement
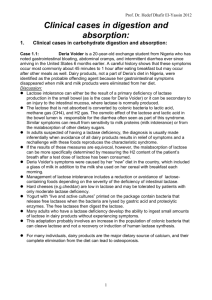
GASTROINTESTINAL VIVAS 2006-2, 2003-2 Describe how proteins are digested in the gastrointestinal tract - Stomach: Proenzyme pepsinogens (secreted by chief cells) are activated by the gastric acid (HCl-, secreted by parietal cells) to produce pepsins and these cleave bonds between amino acids - Small bowel: Proenzymes are secreted by the pancreas and activated in the small intestine - Proteolytic proenzymes from pancreas: Endopeptidases (act at interior peptide bonds, activated at site of action by brush border hydrolase - enterokinase): trypsin(ogen), chymotrypsin(ogen), and (pro)elastase, and note trypsin itself activates these other proenzymes Exopeptidases (cleave side chains at carboxyl ends of polypeptides): (pro)carboxypeptidase A (aliphatic side chains) and B (basic side chains) - Intestinal mucosa has the activating enterokinase (aka enteropeptidase) How are proteins absorbed from the gastrointestinal tract? - Via di- and tri-peptides, very little larger peptides - Rapid in duodenum and jejunum, slow in ileum - 50% from digested food, 25% from proteins in the digestive juices, 25% from desquamated mucosal cells - Only 2-5% escapes digestion in small bowel -> bacteria in large. Protein in stool from bacteria and cellular debris - Two phases: 1. Mucosal cell via 7 transport systems: 5 require Na+, 2 require Na+ and Cl-, and 2 are Na+ independent 2. Interstitial fluid (via 5 transport systems) => capillaries and portal blood - Na+ similar to glucose transport How does protein absorption and digestion differ in infants and young children compared to adult? - Infants absorb more undigested protein (endocytosis => exocytosis) - Results in more food allergy (as high as 8%) but passive immunity (IgAs in maternal colustrum, M cells and Peyer’s patches => IgA and secretory immunity) 2006-1 What factors regulate gastric secretion 3 stimuli of gastric secretion (hormonal x2 and neural) 1. Gastrin - Hormone released by G cells in antrum - In response to neurotransmitter (GRP) and amino acids in gastric lumen - Via bloodstream => fundus: directly on parietal cells w/ release of HCl- (note negative feedback) 2. Histamine: Gastrin also acts on ECL => histamine => H2 receptors on parietal cells => HCl3. ACh – neural stimulation of parietal and chief cells by enteric nerve endings 3 phases of secretion 1. Cephalic: Vagal input from dorsal vagal complex => gastrin releasing peptide (GRP) 2. Gastric: constituents in stomach (e.g. via receptors for amino acids), vaso-vagal stretch, buffering acid w/ loss of negative feedback 3. Intestinal: fats and carbohydrates in duodenum inhibit HCl- and pepsin (by secretin and CCK) Negative feedback: H+ => somatostatin => inhibits G cells (gastrin), ECL cells (histamine), parietal cells (HCl-), H+ also has a direct effect on G cells to decrease gastrin secretion - Peptide YY: inhibits gastric acid secretion and motility (? is the gastric inhibitory peptide) 2010-1, 2005-2 (composition of) Name the principal pancreatic enzymes and the substances upon which they act - The pancreas secretes proenzymes that are activated at required site (95% of proteins in juice) Also contains a trypsin inhibitor to prevent autodigestion In pancreatitis phospholipase A2 is activated (by trypsin) in the ducts Pancreatic juice is alkaline (pH ~8.0) with a high HCO3- content Contains cations (Na+, K+, Ca2+, Mg2+) and anions (HCO3-, SO42-, HPO42-) About 1500ml is secreted per day Enzyme Trypsin(ogen) Chymotrypsin(ogen) (Pro)elastase (Pro)carboxypeptidase A (Pro)carboxypeptidase B (Pro)phospholipase A2 (Pro)colipase Pancreatic lipase Bile salt-acid lipase Pancreatic -amylase Ribonuclease Deoxyribonuclease Substrate Proteins and Polypetides Endopeptidases Activated by Enterokinase in brush border Exopeptidase: Aliphatic side chains Exopeptidase: Basic side chains Phospholipids Fat droplets Triglycerides Cholesterol esters Starch RNA DNA Trypsin Cl- Desribe the regulation of pancreatic juice secretion - Primarily under hormonal control (secretin and CCK, also ACh) Secretin - From S cells in upper small intestine - Acts on the ducts (via cAMP) => copious alkaline juice ( HCO3-) w/ enzymes - As flow of pancreatic juice it becomes more alkaline because exchange of HCO3- for CI- in the distal duct (inversely proportional to flow) - Also stimulates bile secretion, decreases HCl-, and may cause contraction of the pyloric sphincter CCK (cholecystokinin) - From musosal cells in upper intestine - Acts on acinar cells (via phospholipase C) to cause of release of zymogen granules and pancreatic juice rich in enzymes but low in volume - Also stimulates gall bladder contraction (hence the name), inhibits gastric emptying, has a trophic effect on pancreas, and enhances motility in the bowel Acetylcholine also stimulates release of zymogen granules (minor effect ?basis of vagally-mediated pancreatic juice secretion in response to sight/smell of food) 2003-2 Describe the enzymes required for the digestion of carbohydrates and their location Ingested Saliva/pancreas => Brush border Absorbed Polysaccharides Oligosaccharides Oligosaccharidases -amylases (starch) - Maltose (di) - Isomaltase Hexoses - Maltriose (tri) - Maltase (Monosaccharides) - Galactose - -dextrin (poly) - Sucrase - Fructose Disaccharides Disaccharidases - Glucose - Lactose - Lactase - Sucrose - Trehalase Sucrose => Fructose + Glucose, Lactase => Galactose + Glucose, Trehalose and Maltose => Glucose x2 Please describe how carbohydrates are absorbed from the gastrointestinal tract - Hexoses are rapidly absorbed across the wall of the small intestine - Almost all before reaching the terminal ileum - Two phases: first into intestinal mucosal cell and second into interstitial fluid (ECF) and thus into capillaries and portal blood Glucose/Galactose - Undergoes co-transport from the intestinal lumen with Na+ via SLGT-1&2 (a low concentration of lumenal Na inhibits b/c driven by concentration gradient) - The Na+ is actively transported into the lateral intercellular spaces - The glucose moves by facilitated diffusion into the ICF via GLUT-2 - Thus glucose transport is by secondary active transport Fructose - By facilitated diffusion from intestinal lumen by GLUT-5 and then GLUT-2 into ICF 2003-2 Describe the enzymes required for the digestion of lipids and their location - Lingual lipase (Ebner’s Gland): active in the stomach on triglycerides, minimal significant activity - Pancreatic lipase: requires colipase for maximal activity (triglycerides) - Pancreatic bile-salt activated lipase (not only triglycerides but also cholesterol esters, some vitamins & phospholipids) - Cholesteryl ester hydrolase (cholesterol) What other process is involved in the digestion of lipids? - Emulsification: due to the detergent action of bile salts, lecithin and monoglycerides - Micelles: If the concentration is high micelles form with formed from bile salts surrounding fatty acids, monoglycerides and cholesterol – a hydrophilic outer layer and hydrophobic centre - Transport lipids thru “unstirred layer” to brush border of mucosal cells Please describe how lipids are absorbed from the gastrointestinal tract - Two phases: first into intestinal mucosal cell and second into interstitial fluid (ECF) and thus into capillaries and portal blood (FFA – free fatty acids) or into lymphatics (chylomicrons) 1. Into enterocytes: passive diffusion & carriers 2. Out of enterocytes: depending on size (< 10-12 carbons => directly into portal blood (FFA’s) OR > 10-12 carbons => reesterified to triglycerides or cholesteryl esters and packaged in chylomicrons (coating of protein, cholesterol and phospholipids) 2008-1, 2004-2 Please describe how ingested iron is absorbed - Most ingested iron is ferric (Fe3+) but the ferrous (Fe2+) form is absorbed - Minimal absorption in stomach but gastric secretions dissolves iron and aid conversion to the ferrous form - Fe3+ reductase activity is associated with the Fe transporter in the brush border - Almost all absorption in duodenum - Iron is transported into enterocytes via DMT1 - Some stored as ferritin - Remainder transported out via ferroportin 1 (basolateral transporter) in the presence of hephaestin - Then converted to ferric form in plasma and bound to transferrin - Dietary heme is absorbed by an apical transporter and iron is removed from the porphyrin in cytoplasm - Note: 70% of Fe in body is in Hb, 3% in myoglobin, remainder in ferritin (present in eneterocytes and other cells) What are the mechanisms that regulate iron absorption? - Precise mechanisms uncertain, probably related to: - Recent dietary intake of iron - State of body iron stores - State of erythropoiesis in bone marrow - The regulatory mechanisms are unclear Physiologically, how is iron lost from the body? 2004-2 - Gut cells - Menstruation 2009-2, 2006-1 What are the principal functions of the Liver? 1. Bile formation (500 mls a day): Excretion, elimination, digestion 2. Nutrient and vitamin metabolism/control - Glucose and other sugars (glucose buffer function) - Amino acids - Lipids (fatty acids, chlesterol, lipoproteins - Vitamins, both fat and water soluble 3. Inactivation and detoxification - Ammonia metabolism/excretion via the urea cycle - Toxins, steroids, hormones, drugs 4. Synthesis - Acute phase proteins - Albumin - Clotting factors - Binding proteins (steroid and hormone binding) 5. Immunity (particulary gut organisms): Kupffer/Macrophages in sinusoid endothelium Describe bilirubins path from production to excretion - Most formed by breakdown of Heme/Hb by marcphages => biliverdin - Biliverdin rapidly reduces to bilirubin - Bilirubin bound to albumin - In liver actively transported (OATP) as dissociates => binds to cytoplasmic proteins - Conjugated by glucuronyl transferase (in ER) with glucoronic acid to H2O soluble bilirubin diglucuronide - Active transport into bile canaliculi (small amount escape into the blood => urinary excretion) - Thus plasma contains mostly free bilirubin (w/ albumin) and conjugated bilirubin - The bilirubin is delivered in bile to intestines (via bile ducts) - Intestinal mucosa relatively impermeable to conjugated bilirubin - Gut bacteria convert most => urobilinogens (colourless) - Some bile pigments, urobilinogens and unconjugated bilirubin are reabsorbed in portal circulation - Most resecreted => enterohepatic circulation - Small amounts urobilinogens enter the general circulation and are excreted in urine - Small amount are excreted in the stool => stercobilinogen which is oxidized to stercobilin