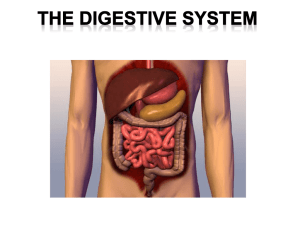
The Digestive System
advertisement

The Digestive System Functions of Digestive System food blood Absorbable nutrients wall lumen Intestines wall digestion food blood Absorbable nutrients wall lumen Intestines wall digestion food blood Absorbable nutrients absorption Forms of Nutrients In Food Absorbable by Intestine Protein Carbohydrates Fat DNA, RNA Vit B12 Amino acids Monosaccharides (glucose) Fatty acids, glycerol Bases + monosaccharides B12+intrinsic factor Other vitamins Cholesterol Electrolytes Water Original form Original form Original form Original form digestion food blood Amino acids Glucose Fatty acids, Glycerol Bases + monosaccharides vitamins Cholesterol Electrolytes, Water absorption The Organs of the Digestive System The Mouth The Salivary Glands The Esophagus The Stomach The Liver The Gallbladder The Pancreas The Small intestines The Large intestines The Mouth has the following functions : 1) breaking food 2) sense of taste 3) swallowing 4) speech Saliva and the Salivary Glands 1) moisten food and the mouth 2) clean the teeth, inhibit bacterial growth, 3) dissolve molecules so they can stimulate taste buds 4) digest a small amount of starch and fat Esophagus Esophagus The Stomach The Stomach Functions - food storage - host defense - minor role in digestion and absorption of nutrients - The above functions are performed via gastric secretion and motility Gastric pits mucous cells: produce The bottom part of mucus the pits is the gastric parietal cells:gland. produce HCl and intrinsic factor chief cells: produce pepsinogen G cells: produce hormones that regulate digestion The gastric glands produce 2-3 L of gastric juice daily, containing: pepsinogen HCl intrinsic factor Pepsinogen - is the inactive precursor of the active enzyme pepsin. - activated by HCl or pepsin. Pepsin: chop proteins into small fragments Pepsinogen Hydrochloric Acid ( HCl ) - reduces pH of gastric juice to as low as pH 0.8. HCl Functions of HCl: (1) activates pepsinogen into pepsin. (2) breaks up connective tissues and plant cell walls. (3) converts ferric ions to ferrous ions. (4) destroys ingested pathogens. HCl Self protection of the stomach from HCl and pepsin by 1) a highly alkaline mucous coat. 2) rapid replacement of epithelial cells (3-6 d) 3) tight junctions between epithelial cells HCl Intrinsic Factor - is essential to the absorption of vitamin B12 - is the only indispensable function of the stomach. Intrinsic Factor Gastrin secreted by G cells in gastric gland not into gastric juice but blood - is a hormone - stimulates 1) the secretion of HCl and pepsinogen 2) motility of the large intestine Gastric Motility - relax during swallowing - stretch further when food enters the stomach (stress-relaxation response) - Next, pacemaker cells in the greater curvature initiate peristaltic contractions. - Each peristaltic wave pushs ~ 3 mL of chyme into the duodenum. Regulation of Gastric Function Gastric secretion and motility is divided into three stages: 1) Cephalic 2) Gastric 3) Intestinal phases 1) The Cephalic Phase The cephalic phase is stimulated by the sight, smell, taste, or mere thought of food. 2) The Gastric Phase - is stimulated by food in the stomach - accounts for two-thirds of gastric secretion. 3) The Intestinal Phase After entering small intestines, chyme inhibit gastric secretion and mobility via: a) the enterogastric reflex. b) local hormones Secretin Cholecystokinin gastric inhibitory peptide The small intestine receives not only chyme from the stomach but also secretions from the liver and pancreas. The Liver has tremendous variety of functions, including the secretion of bile for digestive purposes. Hepatocytes secret bile into the bile canaliculi and bile ductules. bile ductule common Bile ductules hepatic ducts hepatic duct cystic duct common hepatic duct common bile duct gallbladder hepatopancreatic sphincter pancreas duodenum When no chyme is in the small intestine, the hepatopancreatic sphincter is closed. Bile flows into gallbladder. cystic duct common hepatic duct common bile duct gallbladder hepatopancreatic sphincter pancreas duodenum Function of Gallbladder - absorbs water and stores the bile for later use. gallbladder hepatopancreatic sphincter duodenum Bile - is constantly produced by the liver (500-1,000 mL of bile per day). - is a yellow-green fluid containing : minerals bile pigments bile acids phospholipids cholesterol neutral fats facilitate fat digestion and absorption Recycle of Bile acids and Phospholipids - reabsorbed in the ileum and returned to the liver via enterohepatic circulation. Bile acids phospholipids The Pancreas The Pancreas Exocrine: - secretes pancreatic juice into the lumen of the pancreatic duct Endocrine: - secretes insulin, glucagon, somatostatin into the blood. Exocrine secretes 1,200-1,500 mL of pancreatic juice per day into the main pancreatic duct. It empties into duodenum when hepatopancreatic sphincter opens. Pancreatic juice is an alkaline mixture containing: 1) sodium bicarbonate: neutralize HCl 2) inactive digestive enzymes and zymogens which are activated after secreted into duodenum. The activated enzymes digest carbohydrates, lipids, RNA, DNA, and proteins. Regulation of Bile and Pancreatic Secretion - secreted in response to similar stimuli. -Cephalic and Gastric phases The vagus nerves stimulate pancreatic secretion. The Intestinal Phase - Chyme with acid and fat, stimulate the duodenal mucosa to secrete cholecystokinin (CCK). 1) relaxation of the hepatopancreatic sphincter, 2) the contraction of the gallbladder 3) secretion of pancreatic juice and enzymes. The Intestinal Phase - Acidic chyme also stimulates the duodenum to release secretin. secretion of bicarbonate by both the hepatic and pancreatic ducts The Small Intestine Overview - Nearly all chemical digestion and nutrient absorption occur in the small intestines. 1) The duodenum - ~ 25 cm 2) The jejunum - comprises the next 2.5 m. 3) The ileum - forms the last 3.6 m. - The surface area inside the small intestine is greatly increased by circular folds, villi, and microvilli. villi Microvilli (brush border) brush border enzymes brush border enzymes - activates zymogens - complete digestion of carbohydrates and proteins Secretion by the small intestines - 1-2 L of intestinal juice per day. - The duodenum endocrine cells secret cholecystokinin (CCK) and secretin. (Both are hormones.) Chemical Digestion and Absorption of Nutrients Chemical Digestion and Absorption of Nutrients Carbohydrates Proteins Lipids Nucleic Acids Vitamins Minerals Water Digestion and Absorption of Carbohydrate - Most digestible dietary carbohydrate is starch. - The starch digestion begins in the mouth by salivary amylase. - But fully digestion of starch occurs in the small intestines. - Starch is digested to oligosaccharides (3-8 glucose residues), disaccharide maltose, and glucose. pancreatic amylase Brush border enzymes oligosaccharides starch Intestinal lumen glucose glucose glucose Intestinal epithelial cells blood Glucose is absorbed by: - sodium-dependent glucose transporter (SGLT). - solvent drag Digestion and Absorption of Proteins - Proteins are digested by proteases and peptidases. - Protein digestion starts in the stomach. Protein digestion continues in the small intestine by pancreatic enzymes trypsin and chymotrypsin. Protein digestion is completed in the small intestine by brush border enzymes carboxypeptidase, aminopeptidase, and dipeptidase. Amino acid absorption is similar to that of monosaccharides, via several sodium-dependent amino acid cotransporters. Gastric pepsin & pancreatic proteases proteins Brush border enzymes short peptides Intestinal lumen amino acids Intestinal epithelial cells blood Digestion and Absorption of Lipids - Lipids are digested by enzymes called lipases. - Most fat digestion occurs in the small intestine via several steps. 1) Fats are first broken up into smaller emulsification droplets by lecithin and bile salts (acids) in the bile. 2) When lipase digests fats, the products are two fatty acids (FFAs) and a monoglyceride. 3) Bile salts coat these and other lipids and form droplets called micelles. Micelles release their lipids, which diffuse freely across the plasma membrane. Resynthesis of triglycerides. Coating with protein, forming droplets called chylomicrons. Intestinal absorptive cell Chylomicrons are too large to enter blood capillaries and must be first transported in the lymphatic lacteal. Bile salts lipase & bile salts Fat globule emulsification droplets Intestinal lumen chylomicrons micelles Intestinal epithelial cells lacteal blood Digestion and Absorption of Nucleic Acids - The pancreatic nucleases hydrolyze nucleic acids to their component nucleotides. - The brush border nucleosidases and phosphatases further break them down, and the products are transported across the intestinal epithelium by membrane carriers. Absorption of Vitamins - Vitamins are absorbed without digestion. - The fat-soluble vitamins are absorbed with other lipids. - Water soluble vitamins are absorbed by simple diffusion, with the exception of vitamin B12. - Vitamin B12 is an unusually large molecule that can only be absorbed with the help of intrinsic factor. Absorption of Minerals - Minerals (electrolytes) are absorbed without digestion. - Iron and calcium are unusual in that they are absorbed in proportion to the body's need. - Other minerals are absorbed at fairly constant rates regardless of need. Absorption of Water - The digestive tract receives about 9 L of water per day 0.7 L in food 1.6 L in drink 6.7 L in gastrointestinal secretions - ~ 8 L absorbed by the small intestine via osmosis; Intestinal Motility serve three functions: 1) to mix chyme with intestinal juice, bile, and pancreatic juice (segmentation) 2) to churn chyme and bring it in contact with the brush border for digestion and absorption; (segmentation) 3) to move residue toward the large intestine. (peristalsis) - Segmentation is the most common type of movement of the small intestine. - When nutrients have been absorbed, segmentation slows and peristalsis begins. - The intensity of the contractions is modified by nervous and hormonal influences. The Large Intestine - No further chemical digestion - Water (~ 1L) is further absorbed. - The feces consists of: 75% water 25% solid matter, of which 30% is bacteria, and 30% undigested fiber. Bacterial Flora - refer to several species of useful bacteria in large intestine. - ferment cellulose and other undigested carbohydrates - synthesize B vitamins and vitamin K, which are absorbed by the colon. Strong contractions called mass movements occur one to three times a day, last about 15 minutes each, and occur especially an hour after breakfast. Neural Control of Defecation 1. Filling of the rectum 2. Reflex contraction of rectum & relaxation of internal anal sphincter 3. Voluntary relaxation of external sphincter Diarrhea too little water absorbed Constipation too much water absorbed, causing difficulty in defecation In the absence of bile, a fat-rich diet causes diarrhea. Accumulation of fat molecules osmolarity of intestinal content retain water diarrhea People lacking lactase have diarrhea after drinking milk. Lactose (a dimer) lactase glucose galactose People lacking lactase have diarrhea after drinking milk. Accumulation of Lactose osmolarity of intestinal content retain water diarrhea SUMMARY The Organs Digestion and Absorption of Nutrients The Stomach Carbohydrates The Liver Proteins The Gallbladder Lipids The Pancreas Nucleic Acids The Small intestine The Large intestine Vitamins Minerals Water