Leukocytes (White Blood Cells)
advertisement

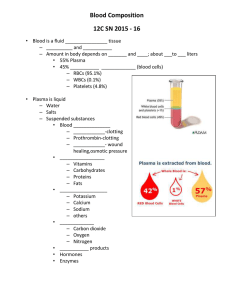
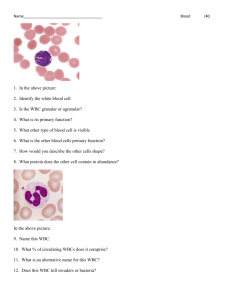
Chapter 33: Resistance of the Body to Infection. I. Leukocytes, Granulocytes, the Monocyte-Macrophage System, and Inflammation Guyton and Hall, Textbook of Medical Physiology, 12th edition Leukocytes (White Blood Cells) • General Characteristics a. Types: neutrophils, basophils, eosinophils, monocytes, lymphocytes (plasma cells) b. Concentrations in the blood White Blood Cell % in Whole Blood Polymorphonuclear Neutrophils 62.0% Polymorphonuclear Eosinophils 2.3% Polymorphonuclear Basophils 0.4% Monocytes 5.3% Lymphocytes 30.0% Leukocytes (White Blood Cells) • Genesis of WBCs Fig. 33.1 Genesis of WBCs Leukocytes (White Blood Cells) • Life Span of WBCs a. Granulocytes- 4-8 hrs in the blood and 4-5 days in tissues b. Monocytes- 10-20 hrs in the blood, move into tissues and become macrophages which can live for months c. Lymphocytes- weeks or months moving from circulation into the tissues and back again d. Platelets- replaced about every 10 days (30,000 formed per day per microliter of blood Neutrophils and Macrophages Defend Against Infections • WBCs Enter the Tissue Spaces by Diapedsis • WBCs Move Through the Tissues by Ameboid Motion • WBCs Are Attracted to Inflamed Tissue by Chemotaxis Neutrophils and Macrophages (cont.) Fig. 33.2 Neutrophils and Macrophages (cont.) • Phagocytosis a. Process b. Neutrophils c. Macrophages d. Phagolysosomes e. Bactericidal properties Monocyte-Macrophage Cells System • Reticuloendothelial System (RES) a. b. c. d. e. Histiocytes Macrophages in the lymph nodes Lungs Kupffer cells Spleen and Bone Marrow Fig. 33.3 Functional diagram of a lymph node Fig. 33.4 Kupffer cells lining the liver sinusoids Fig. 33.5 Functional structures of the spleen Inflammation: Role of Neutrophils and Macrophages • Inflammation a. b. c. d. e. f. Vasodilation of local blood vessels Increased permeability of the capillaries Clotting of fluids in the interstitial spaces Migration of granulocytes and monocytes Swelling of the tissue cells Chemicals released: histamine, bradykinin, serotonin, prostaglandins, complement proteins activated, multiple lymphokines Inflammation: Role of Neutrophils and Macrophages • “Walling-Off” Effect of Inflammation- delay the spread of bacterial or toxins • Macrophage and Neutrophil Responses a. b. c. d. Neutrophil invasion of the inflammed area Acute increase of neutrophils in blood Macrophage invasion into area Increased production of granulocytes and monocytes by the bone marrow Fig. 33.6 Migration of neutrophils from the blood into the inflamed tissue Inflammation (cont.) • Feedback Control of the Macrophage/Neutrophil Responses G-CSF: Granulocyte Colony Stimulating Factor GM-CSF: Granulocyte-Monocyte Colony Stimulating Factor IL-1: Inteleukin 1 M-CSF: Monocyte Colony Stimulating Factor TNF: Tumor Necrosis Factor Fig. 33.7 Eosinophils • Eosinophils a. Weakly phagocytic b. Prominent in parasitic infections c. Collect in areas where allergic reactions occur Basophils • Basophils a. Similar to mast cells b. Release heparin in the blood c. Release histamine, bradykinin, and serotonin d. IgE binds to basophil-release of histamine in allergic reactions Leukopenia and Leukemia • Leukopenia- bone marrow produces few wbcs a. Caused by irradiation (x-rays or gamma rays) b. Exposure to drugs and chemicals • Leukemia- uncontrolled production of wbcs a. Types b. Effects on the body