White blood cells count: A WBC count is a blood test to measure the
advertisement

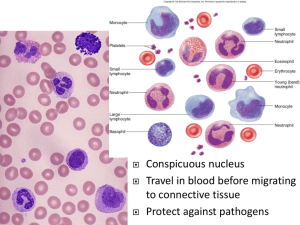
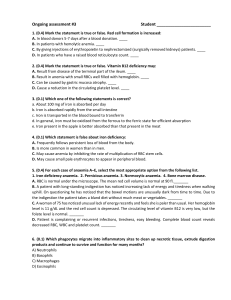
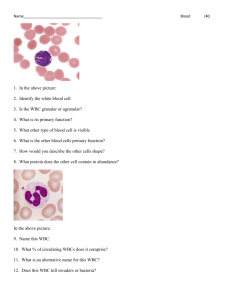
White blood cells count: A WBC count is a blood test to measure the number of white blood cells (WBCs). White blood cells help fight infections. They are also called leukocytes. There are five major types of white blood cells: Neutrophils Lymphocytes (T cells and B cells) Monocytes Eosinophils Basophils Total white blood cells - All the white cell types are given as a percentage and as an absolute number per litre. Neutrophil granulocytes - May indicate bacterial infection. May also be raised in acute viral infections. Neutrophils are phagocytes, capable of ingesting microorganisms or particles. They can internalize and kill many microbes, each phagocytic event resulting in the formation of a phagosome into which reactive oxygen species and hydrolytic enzymes are secreted. The consumption of oxygen during the generation of reactive oxygen species has been termed the "respiratory burst," although unrelated to respiration or energy production. The respiratory burst involves the activation of the enzyme NADPH oxidase, which produces large quantities of superoxide, a reactive oxygen species. Superoxide dismutates, spontaneously or through catalysis via enzymes known as superoxide dismutases (Cu/ZnSOD and MnSOD), to hydrogen peroxide, which is then converted to hypochlorous acid HOCl, by the green heme enzyme myeloperoxidase. It is thought that the bactericidal properties of HOCl are enough to kill bacteria phagocytosed by the neutrophil, but this may instead be step necessary for the activation of proteases. Lymphocytes - Higher with some viral infections such as glandular fever and. Also raised in lymphocytic leukemia. Can be decreased by HIV infection. In adults, lymphocytes are the second most common WBC type after neutrophils. In young children under age 8, lymphocytes are more common than neutrophils. LYMPHOCYTE FUNCTION OF CLASS LYMPHOCYTE Lysis of virally infected cells and NK cells tumour cells Release cytokines and growth factors that regulate other immune Helper T cells cells Lysis of virally infected cells, Cytotoxic T cells tumour cells and allografts Immunoregulation and cytotoxicity γδ T cells Secretion of antibodies B cells PROPORTION 7% (2-13%) 46% (28-59%) 19% (13-32%) 23% (18-47%) Monocytes - May be raised in bacterial infection, tuberculosis, malaria, monocytic leukemia, chronic ulcerative colitis and regional enteritis. Monocyte is a type of white blood cell, part of the human body's immune system. Monocytes have two main functions in the immune system: (1) replenish resident macrophages and dendritic cells under normal states, and (2) in response to inflammation signals, monocytes can move quickly (approx. 8-12 hours) to sites of infection in the tissues and divide/differentiate into macrophages and dendritic cells to elicit an immune response. Half of them are stored in the spleen. Monocytes are usually identified in stained smears by their large bilobate nucleus. Eosinophil granulocytes - Increased in parasitic infections, asthma, or allergic reaction. Basophil granulocytes- May be increased in bone marrow related conditions such as leukemia or lymphoma. Overview table Type Approx .% Microscopic in Diameter Main targets Appearance adults (μm) Blood valu es Nucleus Granules Lifetime Neutrophil 54–62% 10–12 Eosinophil 1–6% 10–12 Basophil <1% 12–15 Macrophage bi-lobed or trilobed large blue ? in allergic reactions B cells: various pathogens T cells: o CD4+(helper): extracellular bacteria broken down into peptides presented by MHC class 2 deeply molecule. staining, o CD8+ eccentric cytotoxic T cells: virusinfected and tumor cells. o γδ T cells: Natural killer cells: virus-infected and tumor cells. 25–33% 7–8 2–8% 8–12 days (circulate for 4–5 hours) parasites in allergic reactions Monocyte bi-lobed full of pinkorange (H&E Stain) Lymphocyte bacteria fungi 6 hours–few fine, faintly days multilobed pink (H&E (days in Stain) spleen and other tissue) 14–17 Monocytes migrate from the bloodstream to other tissues kidney and differentiate into tissue shaped resident macrophages or dendritic cells. 21 (human) Phagocytosis (engulfment and digestion) of cellular debris and pathogens, and stimulation of lymphocytes and other immune cells that respond to the pathogen. NK-cells and weeks to Cytotoxic years (CD8+) Tcells hours to days none activated: days immature: months to years Main function is as an antigen-presenting cell (APC) that activates T lymphocytes. Dendritic cells The Test is Performed Blood is typically drawn from a vein, usually from the inside of the elbow or the back of the hand. The site is cleaned with germ-killing medicine (antiseptic). The health care provider wraps an elastic band around the upper arm to apply pressure to the area and make the vein swell with blood. Next, the health care provider gently inserts a needle into the vein. The blood collects into an airtight vial or tube attached to the needle. The elastic band is removed from your arm. Once the blood has been collected, the needle is removed, and the puncture site is covered to stop any bleeding. In infants or young children, a sharp tool called a lancet may be used to puncture the skin and make it bleed. The blood collects into a small glass tube called a pipette, or onto a slide or test strip. A bandage may be placed over the area if there is any bleeding. The blood sample is sent to a laboratory. A WBC count is almost always done as part of a complete blood count (CBC). Samples A phlebotomist collects the specimen, in this case blood is drawn in a test tube containing an anticoagulant (EDTA, sometimes citrate) to stop it from clotting, and transported to a laboratory. In the past, counting the cells in a patient's blood was performed manually, by viewing a slide prepared with a sample of the patient's blood under a microscope (a blood film, or peripheral smear). Nowadays, this process is generally automated by use of an automated analyzer, with only approximately 30% samples now being examined manually. Manual blood count similar to macrophages Counting chambers that hold a specified volume of diluted blood (as there are far too many cells if it is not diluted) are used to calculate the number of red and white cells per litre of blood. To identify the numbers of different white cells, a blood film is made, and a large number of white cells (at least 100) are counted. This gives the percentage of cells that are of each type. By multiplying the percentage with the total number of white blood cells, the absolute number of each type of white cell can be obtained. The advantage of manual counting is that automated analysers are not reliable at counting abnormal cells. Normal Results 4,500-10,000 white blood cells per microliter (mcL). Abnormal Results Mean A low number of WBCs is called leukopenia. It may be due to: Bone marrow failure (for example, due to infection, tumor, or abnormal scarring) Collagen-vascular diseases (such as lupus erythematosus) Disease of the liver or spleen Radiation therapy or exposure A high number of WBCs is called leukocytosis. It may be due to: Anemia Infectious diseases Inflammatory disease (such as rheumatoid arthritis or allergy) Leukemia Severe emotional or physical stress Tissue damage (for example, burns) Drugs that may increase WBC counts include: Aspirin Chloroform Corticosteroids Heparin Drugs that may lower your WBC count include: Antibiotics Antihistamines Antithyroid drugs Chemotherapy drugs Diuretics Sulfonamides