Approach to the
Jaundiced Patient
Dr. Ümit Akyüz
Yeditepe University
Division of Gastroenterology
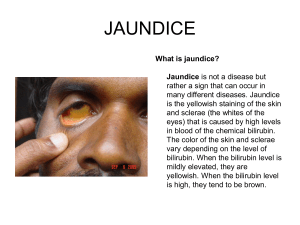
Jaundice
• A yellowing of the skin, sclerae(공막), and
other tissues caused by excess circulating
bilirubin
Bilirubin Metabolism
•
•
•
•
Formation: About 250 to 350 mg of bilirubin forms daily; 70 to 80% derives
from the breakdown of senescent RBCs. The remaining 20 to 30% (earlylabeled bilirubin) comes from other heme proteins located primarily in the
bone marrow and liver. The heme moiety of Hb is degraded to iron and the
intermediate product biliverdin by the enzyme heme oxygenase. Another
enzyme, biliverdin reductase, converts biliverdin to bilirubin.
Plasma transport: Because of internal hydrogen bonding, bilirubin is not
water-soluble. Unconjugated (indirect-reacting) bilirubin is therefore
transported in the plasma bound to albumin
Liver uptake: Uptake of bilirubin is via active transport and is rapid
Conjugation: Free bilirubin concentrated in the liver is conjugated with
glucuronic acid to form bilirubin diglucuronide, or conjugated (directreacting) bilirubin. This reaction, catalyzed by the microsomal enzyme
glucuronyl transferase, renders the bilirubin water-soluble
• indirect reacting bilirubin
The fraction of serum bilirubin which has
not been conjugated with glucuronic acid
in the liver cell; so called because it reacts
with the Ehrlich diazo reagent only when
alcohol is added; increased levels are
found in hepatic disease and haemolytic
conditions.
•
•
Biliary excretion: Conjugated bilirubin is secreted into the bile canaliculus
(모세담관) with other bile constituents. In the intestine, bacterial flora
deconjugate and reduce bilirubin to compounds called stercobilinogens .
The kidney can excrete bilirubin diglucuronide but not unconjugated bilirubin.
This explains the dark urine typical of hepatocellular or cholestatic jaundice
and the absence of urinary bile in hemolytic jaundice
Abnormalities at any of these steps can result in jaundice. Increased
formation, impaired liver uptake, or decreased conjugation can cause
unconjugated hyperbilirubinemia. Impaired biliary excretion produces
conjugated hyperbilirubinemia. In practice, both liver disease and biliary
obstruction create multiple defects, resulting in a mixed
hyperbilirubinemia
Diagnostic Approach to
Jaundice
• Symptoms and Signs
-Mild jaundice without dark urine : unconjugated hyperbilirubinemia
caused by hemolysis or Gilbert's syndrome rather than hepatobiliary
disease
-More severe jaundice or dark urine clearly indicates a liver or biliary
disorder.
-Signs of portal hypertension (문맥고압증), ascites, or skin and
endocrine changes usually imply a chronic rather than an acute
process
-Patients often notice dark urine before skin discoloration; thus, the
onset of dark urine better indicates the duration of jaundice
-Nausea and vomiting preceding jaundice most often indicate acute
hepatitis or common duct obstruction by a stone; abdominal pain or
rigors favor the latter
Laboratory Findings
• Mild hyperbilirubinemia with normal aminotransferase and alkaline
phosphatase levels usually reflects hemolysis or Gilbert's syndrome
rather than liver disease
• Aminotransferase elevations > 500 U suggest hepatitis or an acute
hypoxic episode; disproportionate increases of alkaline phosphatase
suggest a cholestatic or infiltrative disorder
• Low albumin and high globulin levels indicate chronic rather than
acute liver disease
DISORDERS OF BILIRUBIN METABOLISM
• Unconjugated Hyperbilirubinemia :
-Hemolysis
-Gilbert's syndrome : defects in the liver's uptake of
plasma bilirubin (우성유전)
-Crigler-Najjar syndrome : glucuronyl transferase
deficiency
-Primary shunt hyperbilirubinemia: This rare, familial
benign condition is associated with overproduction of
early-labeled bilirubin.
• Noncholestatic Conjugated Hyperbilirubinemia
-Dubin-Johnson syndrome: Asymptomatic mild jaundice
characterizes this rare autosomal recessive disorder.
The basic defect involves impaired excretion of various
organic anions as well as bilirubin, but bile salt excretion
is unimpaired.
-Rotor's syndrome: This rare disorder is similar to DubinJohnson syndrome, but the liver is not pigmented and
other subtle metabolic differences are present
• CHOLESTASIS
-A clinical and biochemical syndrome that results when bile
flow is impaired
• -Etiology :Bile flow may be impaired at any point from the
liver cell canaliculus to the ampulla of Vater(바터팽대부) .
The most common intrahepatic causes are hepatitis,
drug toxicity, and alcoholic liver disease. Less common
causes include primary biliary cirrhosis(담즙성간경변),
cholestasis of pregnancy, metastatic carcinoma, and
numerous uncommon disorders.The most common
extrahepatic causes are a common duct stone and
pancreatic cancer. Less common causes include benign
stricture of the common duct (usually related to prior
surgery), ductal carcinoma, pancreatitis or pancreatic
pseudocyst, and sclerosing cholangitis(경화성 담관염)
-Pathophysiology : interference with microsomal
hydroxylating enzymes, which leads to the formation of
poorly soluble bile acids; impaired activity of Na+,K+ATPase, which is necessary for canalicular bile flow;
altered membrane lipid composition and fluidity;
interference with the function of microfilaments (thought
to be important for canalicular function); and enhanced
ductular reabsorption of bile constituents. Because bile
salts are needed for absorption of fat and vitamin K,
impaired biliary excretion of bile salts can produce
steatorrhea(지방변) and
hypoprothrombinemia(저프로트롬빈혈증 ). In longstanding cholestasis (eg, primary biliary cirrhosis),
concomitant Ca and vitamin D malabsorption may result
in osteoporosis or osteomalacia(골연화증)
• Symptoms and Signs
-Jaundice, dark urine, pale stools, and generalized pruritus(소양증)
• Diagnosis :
-Intrahepatic and extrahepatic cholestasis must be differentiated.
Intrahepatic cholestasis is suggested by symptoms of hepatitis,
heavy alcohol ingestion, recent use of potentially cholestatic drugs,
or signs of chronic hepatocellular disease (eg, spider nevi,
splenomegaly, ascites). Extrahepatic cholestasis is suggested by
biliary or pancreatic pain, rigors(오한), or a palpable gallbladder.
-Laboratory tests
-Imaging studies
-Liver biopsy
• Treatment
-In intrahepatic cholestasis, treating the underlying cause usually
suffices
-Extrahepatic biliary obstruction usually requires intervention: surgery,
endoscopic extraction of ductal stones, or insertion of stents and
drainage catheters for strictures (often malignant) or partially
obstructed areas
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Jaundiced Emergencies
• Acetaminophen Toxicity
• Fulminant Hepatic Failure
• Ascending Cholangitis
Jaundice Unrelated to
Intrinsic Liver Disease
•
•
•
•
•
Hemolysis (usually T. bili < 4)
Massive Transfusion
Resorption of Hematoma
Ineffective Erythropoesis
Disorders of Conjugation
– Gilbert’s syndrome
• Intrahepatic Cholestasis
– Sepsis, TPN, Post-operation
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
HBV Serology
HBSAg HBcAb HBcAb HBSAb
IgM
IgG
Acute HBV
Resolved HBV
Chronic HBV
HBV vaccinated
+
+
-
+
-
+
+
-
+
+
Acute Hepatitis C
Plateau phase = 57 days
HCV
RNA
0
10
20
30
Anti-HCV
40
50
Infection
HCV RNA
HCV Antibody
60
70
Day 0
Day 12
Day 70
From DL Thomas
80
90
100
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Alcoholic Liver Disease
• The history is the key – 60 grams/day
• Gynecomastia, parotids, Dupuytren’s
• Lab clues: AST/ALT > 2, MCV > 94
AST < 300
• Alcoholic hepatitis:
– Anorexia, fever, jaundice, hepatomegaly
– Treatment:
• Abstinence
• Nutrition
• Consider prednisolone or pentoxifylline
Alcoholic Liver Disease
Discriminant Function Formula:
DF = [4.6 x (PT – control)] + bilirubin
Consider treatment for DF > 32
• Prednisolone 40 mg/day x 28 days
– contraindications: infection, renal failure, GIB
• Pentoxifylline 400 mg PO tid x 28 days
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Autoimmune Hepatitis
• Widely variable clinical presentations
– Asymptomatic LFT abnormality (ALT and AST)
– Severe hepatitis with jaundice
– Cirrhosis and complications of portal HTN
• Often associated with other autoimmune dz
• Diagnosis:
– Compatible clinical presentation
– ANA or ASMA with titer 1:80 or greater
– IgG > 1.5 upper limits of normal
– Liver biopsy: portal lymphocytes + plasma cells
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Drug-induced Liver Disease
• Hepatocellular
– acetaminophen, INH, methyldopa, MTX
• Cholestatic
– chlorpromazine, estradiol, antibiotics
• Chronic Hepatitis
– methyldopa, phenytoin, macrodantin, PTU
• Hypersensitivity Reaction
– Phenytoin, Augmentin, allopurinol
• Microvesicular Steatosis
– amiodarone, IV tetracycline, AZT, ddI, stavudine
Acetaminophen Toxicity
• Danger dosages (70 kg patient)
– Toxicity possible > 10 gm
– Severe toxicity certain > 25 gm
– Lower doses potentially hepatotoxic in:
• Chronic alcoholics
• Malnutrition or fasting
• Dilantin, Tegretol, phenobarbital, INH, rifampin
• NOT in acute EtOH ingestion
• NOT in non-alcoholic chronic liver disease
Acetaminophen Toxicity
• Day 1:
– Nausea, vomiting, malaise, or asymptomatic
• Day 2 – 3:
– Initial symptoms resolve
– AST and ALT begin to rise by 36 hours
– RUQ pain, tender enlarged liver on exam
• Day 4
– AST and ALT peak > 3000
– Liver dysfunction: PT, encephalopathy, jaundice
– Acute renal failure (ATN)
Acetaminophen Toxicity
Treatment
• Activated charcoal if < 4 hours from ingestion
– Administer as a single dose 1 mg/kg PO or NG
– Does not adversely effect NAC efficacy
• N-Acetylcysteine (NAC)
– 140 mg/kg loading dose PO or NG
– 70 mg/kg q 4 hours PO or NG X 17 doses
• Continue longer until INR < 2.0 and improved
• OK to DC if acetaminophen levels undetectable
and normal AST at 36 hours
Fulminant Hepatic Failure
• Definition:
– Rapid development of hepatic dysfunction
– Hepatic encephalopathy
– No prior history of liver disease
• Most common causes:
– Acetaminophen
– Unknown
– Idiosyncratic drug reaction
– Acute HAV or HBV (or HDV or HEV)
Fulminant Hepatic Failure
•
•
•
•
Close glucose monitoring
IV glucose
Avoid sedatives - give PO lactulose
Avoid nephrotoxins and hypovolemia
Vitamin K SQ
– Do not give FFP unless active bleeding,
since INR is an important prognostic factor
• GI bleed prophylaxis with PPI
• Transfer all patients with FHF who are
candidates to a liver transplant center
5,6741 Liver Transplants in 2003
Indications:
•
•
•
•
•
•
•
•
•
•
Hepatitis C
Alcoholic Liver Disease
Cirrhosis of unknown etiology
Hepatocellular Carcinoma
Fulminant Hepatic Failure
Primary Sclerosing Cholangitis
Primary Biliary Cirrhosis
Metabolic Liver Disease
Autoimmune Hepatitis
Hepatitis B
29%
15%
8%
7%
6%
5%
4%
4%
3%
3%
Liver Transplantation:
Contraindications
• ABSOLUTE
– active alcohol or drug abuse
– HIV positivity
– extrahepatic malignancy
– uncontrolled extrahepatic infection
– advanced cardiopulmonary disease
• RELATIVE
– Age over 65
– poor social support
– poorly controlled mental illness
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Obstructive Jaundice
CBD stones (choledocholithiasis) vs. tumor
• Clinical features favoring CBD stones:
– Age < 45
– Biliary colic
– Fever
– Transient spike in AST or amylase
• Clinical features favoring cancer:
– Painless jaundice
– Weight loss
– Palpable gallbladder
– Bilirubin > 10
Ascending Cholangitis
• Pus under pressure
• Charcot’s triad: fever, jaundice, RUQ pain
– All 3 present in 70% of patients, but fever > 95%
– May also present as confusion or hypotension
• Most frequent causative organisms:
– E. Coli, Klebsiella, Enterobacter, Enterococcus
– anaerobes are rare and usually post-surgical
• Treatment:
– Antibiotics: Levaquin, Zosyn, meropenem
– ERCP with biliary drainage
Ascending Cholangitis
Indications for Urgent ERCP
•
•
•
•
•
Persistent abdominal pain
Hypotension despite adequate IVF
Fever > 102
Mental confusion
Failure to improve after 12 hours of
antibiotics and supportive care
Obstructive Jaundice
Malignant Causes
• Cancer of the Pancreas
• Cancer of the Bile Ducts
(Cholangiocarcinoma)
• Ampullary Tumors
• Portal Lymphadenopathy
New Onset Jaundice
•
•
•
•
•
•
•
•
Viral hepatitis
Alcoholic liver disease
Autoimmune hepatitis
Medication-induced liver disease
Common bile duct stones
Pancreatic cancer
Primary Biliary Cirrhosis (PBC)
Primary Sclerosing Cholangitis (PSC)
Primary Biliary Cirrhosis
• Cholestatic liver disease (ALP)
– Most common symptoms: pruritus and fatigue
– Many patients asx, and dx by abnormal LFT
• Female:male ratio 9:1
• Diagnosis:
– Compatible clinical presentation
– AMA titer 1:80 or greater (95% sens/spec)
– IgM > 1.5 upper limits of normal
– Liver biopsy: bile duct destruction
• Treatment: Ursodeoxycholic acid 15 mg/kg
Primary Sclerosing Cholangitis
• Cholestatic liver disease (ALP)
• Inflammation of large bile ducts
• 90% associated with IBD
– but only 5% of IBD patients get PSC
• Diagnosis: ERCP (now MRCP)
– No autoantibodies, no elevated globulins
– Biopsy: concentric fibrosis around bile ducts
• Cholangiocarcinoma: 10-15% lifetime risk
• Treatment: Liver Transplantation
Diagnosis of
Immune-Mediated Liver Disease
LFT
Serology Quantitative
Biopsy
Immunoglobulins
AIH
ALT
ANA
ASMA
IgG
Portal
inflammation
Plasmacytes
Piecemeal
necrosis
Bile duct
destruction
granulomas
Periductal
concentric
fibrosis
PBC
ALP
AMA
IgM
PSC
ALP
none
normal
Unusual Causes of Jaundice
•
•
•
•
•
•
•
Ischemic hepatitis
Congestive hepatopathy
Wilson’s disease
AIDS cholangiopathy
Amanita phalloides (mushrooms)
Jamaican bush tea
Infiltrative diseases of the liver
– Amyloidosis
– Sarcoidosis
– Malignancy: lymphoma, metastatic dz
Wilson’s Disease
• Autosomal recessive – copper metabolism
• Chronic hepatitis or fulminant hepatitis
• Associated clinical features:
– Neuropsychiatric disease
– Hemolytic anemia
• Physical exam: Kayser-Fleischer rings
• Diagnosis: ceruloplasmin, urinary Cu
• Treatment: d-penicillamine
Critical Questions in the Evaluation
of the Jaundiced Patient
• Acute vs. Chronic Liver Disease
• Hepatocellular vs. Cholestatic
– Biliary Obstruction vs. Intrahepatic Cholestasis
• Fever
– Could the patient have ascending cholangitis?
• Encephalopathy
– Could the patient have fulminant hepatic failure?
Evaluation of the Jaundiced Patient
HISTORY
•
•
•
•
•
•
•
Pain
Fever
Confusion
Weight loss
Sex, drugs, R&R
Alcohol
Medications
•
•
•
•
•
•
•
•
•
pruritus
malaise, myalgias
dark urine
abdominal girth
edema
other autoimmune dz
HIV status
prior biliary surgery
family history liver dz
Evaluation of the Jaundiced Patient
PHYSICAL EXAM
•
•
•
•
•
•
•
•
BP/HR/Temp
Mental status
Asterixis
Abd tenderness
Liver size
Splenomegaly
Ascites
Edema
•
•
•
•
•
•
Spider angiomata
Hyperpigmentation
Kayser-Fleischer rings
Xanthomas
Gynecomastia
Left supraclavicular
adenopathy
(Virchow’s node)
Evaluation of the Jaundiced Patient
LAB EVALUATION
•
•
•
•
•
•
•
•
AST-ALT-ALP
Bilirubin – total/indirect
Albumin
INR
Glucose
Na-K-PO4, acid-base
Acetaminophen level
CBC/plt
•
•
•
•
•
•
•
Ammonia
Viral serologies
ANA-ASMA-AMA
Quantitative Ig
Ceruloplasmin
Iron profile
Blood cultures
Evaluation of the Jaundiced Patient
• Ultrasound:
– More sensitive than CT for gallbladder stones
– Equally sensitive for dilated ducts
– Portable, cheap, no radiation, no IV contrast
• CT:
– Better imaging of the pancreas and abdomen
• MRCP:
– Imaging of biliary tree comparable to ERCP
• ERCP:
– Therapeutic intervention for stones
– Brushing and biopsy for malignancy
Yes
Treat
Yes
Treat