liver diseases
advertisement
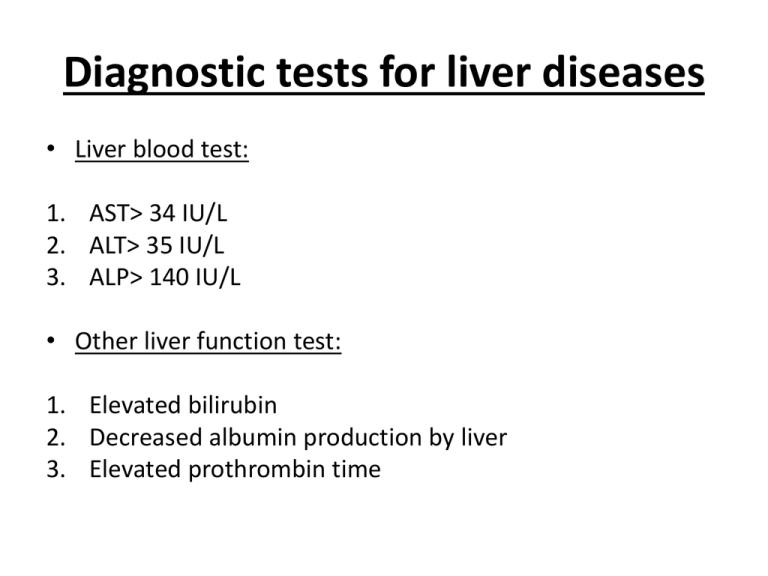
Diagnostic tests for liver diseases • Liver blood test: 1. AST˃ 34 IU/L 2. ALT˃ 35 IU/L 3. ALP˃ 140 IU/L • Other liver function test: 1. Elevated bilirubin 2. Decreased albumin production by liver 3. Elevated prothrombin time Clinical case 1 • A 76-year-old man with a history of COPD was prescribed a course of co-amoxiclav 375 mg three times a day for 7 days. • He presented to his primary care doctor with general malaise, vomiting and pruritus Clinical case 1 Questions • Do the clinical signs in this patient suggest liver disease ? • Is co-amoxiclav a possible cause of liver disease? What other information is required? • What treatment is appropriate? Answer to Clinical case 1 1. General malaise, tiredness and nausea and vomiting are possible signs of liver disease Pruritus is associated with chlestatic jaundice as the bile salts are deposited in the skin and cause itching. 2. co-amoxiclav is a likely cause here, although a complete history is required to exclude other drugs or causes of illness or pre-existing liver disease. 3. -Symptomatic treatment of the itch with antihistamines is appropriate. - Topical treatment with menthol in aqueous cream may provide relief for some patients -Colestyramine may be added Clinical case 2 • A 56 year old man with alcoholic cirrhosis is admitted to hospital following a haematemesis. • He has been abstinent from alcohol for 18 months and is on a waiting list for a liver transplantation because of intractable ascites. • Endoscopy confirms he is bleeding from oesophageal varices which are banded. • The patient is transferred 8 hours later to a specialist regional centre at their request for further management. Clinical case 2 • Laboratory data on admission are: 1. 2. 3. 4. 5. 6. 7. 8. 9. Na K Creatinine Urea Bilirubin ALT PT Albumin Hb 124 (133-143mmol/L) 3.0 (3.5-5.0mmol/L) 131 (80-124µmol/L) 14.3 (2.7-7.7mmol/L) 167 (3.15µmol/L) 24 (0-35 iu/L) 18.9 seconds (13 seconds) 24 (35-50g/dL) 8.9 (13.5-18g/dL) • Drugs on admission: Spironolactone 200 mg one each morning • Q: What treatment would be recommended before the patient is transferred to the regional centre? Answer to Clinical case 2 1. Restore blood volume: colloid then cross matched blood 2. Hypokalemia: dextrose 5% and potassium 3. Reduce portal pressure: terlipressin or octreotide 4. Broad spectrum antibiotics 5. If bleeding from gastric mucosal lesion: give PPI or H2R blockers 6. Spironolactone should be stopped 7. Vit K 8. Encephalopathy may occur so give: lactulose or phosphate enema Clinical case 3 • An 80-year-old African American female (AAF) with a past medical history (PMH) of osteoarthritis (OA) is admitted to the hospital with a chief complaint (CC) of jaundice for 2 months. • The patient did not notice the jaundice or felt any differently but her physician was worried and she was admitted to a different hospital 2 months ago. • The liver ultrasound (U/S) showed gallstones and she had a laparoscopic cholecystectomy 2 months ago. • After surgery, the jaundice decreased slightly but then returned. Clinical case 3 • Past medical history (PMH): -Osteoarthritis (OA), -esophagogastroduodenoscopy (EGD) and colonoscopy 4 months ago were both reported as normal. • Medications: 1. Celebrex (celecoxib), 2. Arthrotec (diclofenac and misoprostol), 3. aspirin (ASA) • Family medical history (FMH): Hypertension (HTN) • Social history (SH): She quit drinking and smoking 40 years ago. Clinical case 3 Questions: 1) What do you think is the cause of the jaundice? 2) What did we learn from this case? Answer to clinical case 3 1. Drug-induced hepatitis due to diclofenac (Arthrotec is diclonefac/misoprostol). 2. Always consider drug-induced hepatitis in your differential diagnosis of hepatitis and jaundice. NSAIDs are among the common causes of LFTs elevation.