jaundice (27th January) - Back to Medical School
advertisement
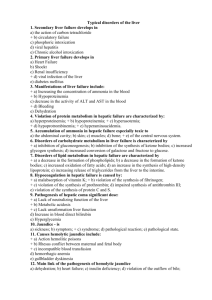
Jaundice and its Investigation Andrew M Smith Jan 2011 Jaundice "it looks like there's something wrong… ….with your television set.“ Matt Groenig, creator of The Simpsons Jaundice • An elevation of serum bilirubin above normal limit (9 mmol/l) • Clinically evident at ~ 35 mmol/l Objectives • Review Liver Anatomy and Physiology • Classification and causes of Jaundice • Investigation of Jaundice • Principles of Management of Jaundice • Cases • Summary Gross Hepatic Anatomy Liver Histological Structure Functions of the Liver 1.Metabolism • • • • Fats Proteins Carbohydrates Hormones 2.Storage 3.Metabolism and excretion bilirubin 4. Drug metabolism and excretion Normal Bile Physiology • 250-500 mg bile/day • • • • • • Water (98%) Bile Salts Bile pigments (Bilirubin) Fatty Acids Lecithin Cholesterol Normal Bilirubin Metabolism RBC Hb Degraded to Globin + Fe + Bilirubin Hepatocyte Bilirubin bound to albumin Conjugated Bilirubin Diglucuronide Kidney Portal Vein Intestine Urobilinogen Urobilinogen Bilirubin Urobilinogen Stercobilin Major Causes of Jaundice Pre-hepatic Haemolysis Ineffective erythropoiesis Hepatic Prematurity Gilberts Drugs Hepatitis: viral, NASH Alcohol / cirrhosis Tumours Extrahepatic sepsis Post-hepatic ‘Obstructive’ Gallstones (in the lumen) Bile duct stricture ( in the wall) Ca pancreas (extrinsic) Investigation Of A Jaundiced Patient • History • Examination • Tests – Blood – Urine – Imaging History ‘most important part of the evaluation of the patient with jaundice’ History 1. Jaundice – onset 2. Pale stools, dark urine? YES = POST HEPATIC PAIN? YES Colicky Fatty food intolerant NO Wt loss Back Pain Non-specific symptoms GALLSTONES MALIGNANCY ASSOCIATED FEVERS / RIGORS? Gram –ve Septicaemia ADMIT NO = PRE & HEPATIC Pre-hepatic: Family history of bleeding disorders, tendency to bleed Hepatic: IV Drug abuse blood transfusions Travel flu-like illness Hepatitis Excess alcohol intake Cirrhosis/ Obesity NASH Drug History Examination • Stigmata Chronic Liver disease • Hepatomegaly – texture,edge, nodules • Hepatosplenomegaly • Ascites –shifting dullness • Portal hypertesion • Obvious iv drug use Examination – obstructive jaundice • Temp • Tachycardic +/- hypotensive • Cachexia, Virchow’s node,clubbing • Murphy’s sign • Courvoisier’s law ‘If in the presence of jaundice the gallbladder is palpable then the cause of the jaundice is unlikely to be gallstones’ • Urine cholangitis Investigations for jaundice • Bloods – General – Liver Function Tests - Albumin, INR (give more info on function!) – Specific • Urine • Imaging • Histology Ix Jaundice – Bloods • Liver Function Tests - really a test of hepatocyte damage Alanine Transaminase ALT range <40iu/L elevated cellular damage AlkalinePhosphatase ALP range 70-300iu/KL elevation post hepatic obstruction Bilirubin range 5- 40 umol/L Prehepatic • Unconguated Bil ↑ • LFT’s N • • • • haptoglobins ↓ Reticulocytes ↑ Coombs test +ve Clotting screen • Urine urobilinogen↑ Hepatic • • • ALT ↑ ↑ ↑ ALP N or ↑ Bil ↑ • • Albumin ↓ INR ↑ • • Hepatitis serology Autoantibodies • • • Caeruloplasmin ↑ • • Anti-mitochondrial PBC Anti-nuclear & antimicrosomal, Autoimmune hepatitis Wilson’s γ-Globulins ↑ • Cirrhosis esp autoimmune • Transferrin ↑ ↑ • α-foetoprotein, αFP ↑ • • Haemochromatosis ↑ HCC in cirrhosis Post - hepatic • ALT N or ↑ • ALP ↑ ↑ ↑ • Bil ↑ • INR ↑ • CEA, Ca19.9 ↑ • Panc & cholangio Ca Imaging - Ultrasound • Key investigation • Distinguish hepatic and post hepatic • Identify gallstones Imaging - Ultrasound Key information from report BILIARY DUCT DILATION Calculi Gallstones present, GB wall thickness CBD diameter normal (<7mm) No calculi No gallstones, but CBD ↑ ? Pancreatic malignancy NO DUCT DILATION Texture of liver eg normal, fatty, micronodular Lesions present Imaging - CT Scan Imaging MRCP + MRI Imaging - Endoscopic ultrasound CBD CBD PD PD Imaging ERCP Imaging PET scan Investigation Summary • First line • LFT’s & USS • Second line – If dilated ducts refer for stone or ? maligancy management – No ducts – parenchymal liver disease – – – – Ensure good alcohol history Hepatitis serology Hepatic autoantibodies Ferritin Case 1 • A 18 year old student comes to see you and reveals that his mates taunt him as he often appears to have yellow eyes? • What do you do? Gilbert’s disease • Diagnosis of exclusion • Good Hx. No family hx of sickle/G6PD defficiency • no other risk factors • Notes jaundice worsens on fasting • Unconguated Bil ↑ and LFT’s N • haptoglobins Reticulocytes both normal, Coombs test ve 5 -7 % population, reasssure. Case 2 • A Samuel Smiths delivery man who enjoys the companys perks to excess attends, complaining of a distended abdomen which is becoming painful? • Diagnosis? • Management? Decompensated alcoholic cirrhosis History – confirms 100+ unit intake for 20 yrs Examination – stigmata chronic liver disease abdo, palpable liver and spleen shifting dullness Ix - LFTs Bil ↑ , ALT ↑ ↑ ↑, ALP ↑ INR ↑ Albumin low USS , cirrhosis, splenomegaly and ascites Treatment – Cessation of alcohol - treatment of withdrawal - thiamine, folic acid - low salt diet, spironolactone - Liver bx when ascites settles - Ix portal htn, OGD, banding, B –blocker, TIPs Case 3 • You are asked to make a home visit to see a 53 yr old man with severe abdominal pain . His notes show that he had an episode of pancreatitis on holiday in Spain a year ago. • He tells you that the has had upper tummy pain, can’t get comfortable and has had shakes and feels cold? • What is the diagnosis? • What action do you take? Ascending Cholangitis • Examination reveals fever, jaundice and a tachycardia. • He has Charcot’s triad – pain, jaundice, fever, ie ascending cholangitis • He needs an emergency admission, significant morbidity and mortality • iv access, analgesia Ascending Cholangitis At hospital, continue resuscitation, antibiotics, check and correct INR Emergency ERCP and duct clearance Laparoscopic Cholecystectomy, same admission Gallstones • Previous pancreatitis due to gallstones. 20% incidence of further complications within 6 months once symptomatic • In elective situation can avoid ERCP, by performing a duct exploration at the time of laparoscopic cholecystectomy • On horizon of further sea change with advent of NOTES (natural orifice transluminal endoscopic surgery) Case 4 • A 37 year old Chinese immigrant who has just arrived in Leeds, presents frankly jaundiced with a history of abdominal pain and weight loss. On examination he is clearly jaundiced and has a palpable liver. • What do we do next? • Can we make an educated guess from the history? Hep C and HCC • LFT’s and USS – ALT, ALP and Bilirubin grossly elevated. • USS cirrhosis and multiple lesions. Referred. • CT and Hep C, aFP Beyond transplant or resection Rx Chemoembolisation / BSC Case 5 Your senior partner has been seeing for a year a previously fit 43yr old man with non specific symptoms of fatigue. Two consecutive ALT’s six months apart were elevated at 120, and 107 ( normal < 40). The rest of his blood work was normal. Do you act on this result? Investigation isolated abnormal LFT Investigation isolated raised ALT • • Present > 6 months should investigate Good Hx and Exam FIRST WAVE TESTS 1 .Exclude drugs NSAIDs, antibiotics, statins, antiepileptic drugs anti-TB. Herbal remedies. Paracetamol 2. Assess Alcohol excess 3. Hep B and C 4. Hereditary Haemochromotosis 5. NASH and steatosis SECOND WAVE TESTS Refer 6. Thyroid/Coeliac/muscle disorders THIRD WAVE – Definitely refer What is the most likely cause of jaundice that I will see? • South Wales, Gut 2002 Glasgow, Gut, 2002 Alcoholic liver disease Gallstones Malignacy Summary • • • • Good history will direct rest of care LFTs and USS initially Admit cholangitis when suspected Admit for symptom control Hep B • Send hepatitis serlogy . • Will assess status to determine whether immune/carrier or chronic infection • HepBsAg, HepBsAb, HepBcAb • chronic infection HepBsAG +ve + HepBcAb +ve • immune • HBV DNA HepBsAb +ve , HepBcAb +ve Hep C • Hep C Antibody • Then Hep C RNA, Hep C genotype and liver biopsy Haemochromotosis • • • • • Frequency 5/1000 Fe and TIBC, Fe saturation > 45% then ferritin Ferritin > 400ng/ml Liver biopsy NASH • NASH more common women and type 2 Diabetes • Hep B/C/HCC negative USS to look for steatosis • Bx if stigmata chronic liver disese Isolated Hyperbilirubinaemia • Occurs – excess production or impaired uptake • Check conjugated vs unconjugated • Assess Haemolysis • No haemolysis, fluctuating bilirubin – gilberts disease. Isolated Alkaline Phosphatase • Source – liver and bone • Increased 3rd trimester and in women between 30 and 50 yrs • Determine source, gGT and 5’nucleosidase increases in bone disease • Gel electrophoresis • If Hepatic – USS, if no obstruction then AMA for PBC • Repeat the LFTs