Testing for urine targets and outcomes
advertisement

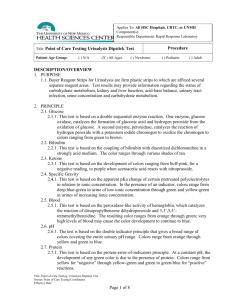
REAGENT STRIPS Storage – – – – – Protect from moisture and excessive heat. Store at room temp. Do not refrigerate. Keep container tightly capped. Do not remove desiccant from container. Do not use beyond expiration date. Handling – Review manufacturer’s instructions with each new lot number – Remove strips from bottle for immediate use. Recap. – Check for discoloration. – Keep away from bleach, acids, fumes, etc. REAGENT STRIPS (continued) • Testing – – – – – – – – – – – within 30 minutes to 2 hours fresh, well-mixed, unspun at room temperature Do not touch test pad area Dip briefly, but completely - app. 1 second Drain off excess urine, avoid runover Do not lay strip on bench Compare test areas to color chart on bottle Read at specified times Know sources of error, interfering substances, sensitivity, and specificity for each strip. When automated, follow instrument’s operating manual. Reporting • Standard terms must be used – Quantitative • Concentration mg/dL • Plus system – Qualitative • Small, moderate, large • Negative/positive/WRR (normal) pH • The strip contains the indicators methyl red and bromthymol blue. The give colors over the pH range of 5-9. Colors range from orange through yellow and green to blue. • Reference value on normal diet - 4.6 to 8.0 CLINICAL SIGNIFICANCE pH Acid pH <6.0 – Diet (high protein, meat, cranberries) – Acidifying drugs to prevent alk. stone formation – Abnormal crystalluria (bilirubin, cystine, tyrosine, leucine, cholesterol ) – Uric acid stone formers – Acidosis and uncontrolled Diabetes mellitus – Hypokalemia – Starvation pH (continued) • Alkaline pH >6.5 – Diet (vegetarian and citrus fruits) – Alkaline tide produced after a meal – Metabolic and respiratory alkalosis – Renal tubular diseases (Fanconi’s syndrome) – Alkalizing drugs to treat acid calculi formation – Genitourinary tract infections • pH >8.0 – Contamination or old urine (not suitable for testing) Protein • Reagent strip testing is based on the principle of protein error of the indicators. Protein in the form of albumin accepts ions from the indicator, which is buffered in a very acid medium. Color changes from shades of green to blue. • Most significant for early detection of renal disease. CLINICAL SIGNIFICANCE PROTEIN • Reference value – – Random urine negative (not detectable) <10mg/dL) 24 Hour <150mg or 10 mg/dL • Composition – – Albumin, 1/3a Globulins, 2/3 • Tamm-Horsfall mucoprotein (25%) • Pathology >30mg/dL or on daily output – – – Heavy >3g/day Moderate >1-3 g/day Minimal <1g/day CLINICAL SIGNIFICANCE PROTEIN (CONTINUED) • Benign – Functional • – Orthostatic • – exercise, fever, stress, exposure to cold positional, renal congestion Pregnancy • transient, investigate cause • Pathologic – Prerenal: overflow of low mole weight proteins • • • IgG light chains (Bence Jones proteins) acute phase hemoglobin, myoglobin CLINICAL SIGNIFICANCE PROTEIN (CONTINUED) • Pathologic – Renal Glomerular Pattern • • • – Renal Tubular Pattern • • • – Group A strep and SLE glomerulonephritis Hypertensive and diabetic nephropathy Nephrotic syndrome, tumors, infections, toxic agents Acute and chronic pyelonephritis Interstitial nephritis Renal tubular acidosis, rejection of kidney transplant Post Renal • Inflammation/infection bladder, renal pelvis, ureter, prostate, external genitalia SSA Testing for Protein • When mixed with weak sulfosalicylic acid (SSA), all urine proteins will denature and precipitate at room temperature. The degree of which is graded and reported in semi-quantitative terms. – Albumin, globulins, glycoproteins, and Bence-Jones protein are detected. – False positive caused by x-ray contrast media, penicillin, sulfonamides, tolbutamides – False negative caused by highly alkaline urine Microalbuminuria • Protein (albumin) that cannot be detected by routine dipstick for protein – Sensitive methods needed to detect 10-20mg/L or 12 mg/dL • Immunochemical • Dye binding • Clinical significance – Early management of kidney disease in diabetes, hypertension, or peripheral vascular disease Glucose • The dipstick determination of glucose is based on a double sequential enzymatic reaction using the specific glucose oxidase/peroxidase reaction in the presence of glucose and a chromogen. • The Clinitest or Benedict’s Reaction is based on the ability of reducing substances to reduce copper sulfate to cuprous oxide in the presence of a chromogen, which changes color from blue to orange. Test is performed to screen for non-glucose reducing sugars in infants and children under 2 years old. Clinical Significance of Glucose • Reference value – No detectable amount present in urine by dipstick method (<50 mg/dl) • Positive values found when renal threshold for glucose is exceeded (160-180 mg/dl) – Diabetes mellitus (DM) – Impaired tubular reabsorption – Pregnancy with latent DM COMPARISON of REAGENT STRIP vs. CLINITEST Strip Clinitest Positive Negative Negative* Positive Cause Sensitivity of methods Oxidizing contaminants/bleach Deteriorated Clinitest tablets Non-glucose reducing substance Deteriorated reagent strips Reagent strip interferences *Ascorbic acid (vitamin C) Ketones • Conditions that result in increased and or incomplete fat metabolism can produce metabolic intermediary fat products in the urine and blood. The three ketone bodies present in urine are acetoacetic acid (20%), acetone (2%), and betahydroxybutyric acid (78%). • Acetoacetic acid and acetone react with nitroprusside in an alkaline medium to form a violet dye complex. Basis of dipstick. • Betahydroxybutyric acid is not detected with dipstick. Clinical Significance Acetone • No detectable ketones present in normal urines. • Positive values – Diabetic ketosis (ketonuria) – Loss of carbohydrates due to fever, vomiting, weight loss, starvation, diarrhea, stress – Lactic acidosis caused by liver/renal failure, salicylate overdose • Interfering factors – False positive: pigmented urines – False negative: delay in testing Nitrite • This test depends on the conversion of nitrate to nitrite by the action on Gram negative bacteria that contain reductase enzymes in the urine. • At the acid pH of the reagent area, nitrite in the urine reacts with an aromatic amine to form a diazonium salt, followed by a coupling reaction with benzoquinoline to produce a pink color. • Three factors must be present – Reductase producing bacteria must be present – Urine must be retained in bladder long enough to convert nitrates to nitrites (4 hours) – Nitrates must be present CLINICAL SIGNIFICANCE NITRITE • Reference value – No nitrites present – Urine must be FRESH – Improper storage will result in false positive • Positive nitrites – Screen symptomatic and asymptomatic UTI – Common infecting organisms • – Enterobacter, Citrobacter, Escherichia, Proteus, Klebsiella, Pseudomonas Definitive diagnosis made by urine culture • Non-reductase producing microorganisms will be negative for nitrites Leukocyte Esterase • Granulocytic leukocytes contain esterase activity that catalyze the hydrolysis of an amino acid ester to form an aromatic compound which reacts with a diazonium salt to produce a color change from beige to purple on the dipstick pad. • All positive reactions require a microscopic exam of the sediment. CLINICAL SIGNIFICANCE LEUKOCYTE ESTERASE • Reference value – 0-5 white cells/hpf – females 0-8 WBC/hpf or app. 10 WBC/uL (vaginal discharge can cause false positive) • Screens for urinary tract inflammation – – – kidney (pyelonephritis) bladder (cystitis) urethra (urethritis) • Leukocyturia can occur with or without bacteria LEUKOCYTE-NITRITE Combination on FRESH urine is • Cost effective tool to screen for UTI • Provides 97% predictive value for negative culture when both tests are negative • Improved care in asymptomatic patient Blood • Dipstick will detect blood by sensing heme that is present in red cell, hemoglobin, and myoglobin. Based on the pseudoperoxidase activity of heme in the presence of an organic peroxide and a benzidine chromogen. – Hematuria: in tact red cells present in urine (scattered green dots) – Hemoglobinuria: presence of hemoglobin from lysed red cell in urine (diffuse green color) – Myoglobinuria: presence of heme protein from muscles in urine (diffuse green color) CLINICAL SIGNIFICANCE BLOOD • Reference value – 0-5 erythrocytes/mL or 0-2 RBC/hpf • Hematuria - intact red cells – – renal disease, calculi, tumors, infections bleeding in kidneys or lower urinary tract • Hemoglobinuria - free hemoglobin – intravascular hemolysis as seen in incompatible blood transfusions, AIHA, G6PD, etc. • Myoglobinuria - heme muscle protein – – acute destruction of muscle fibers (rhabdomyolysis) crush/trauma injuries • Excessive exercise can cause all above COMPARISON of URINE FINDINGS Findings Hematuria Hemoglobinuria Myoglobinuria Color pink, red, smoke clear pink, red, brown clear red, brown UA Blood strip positive dots positive diffuse positive diffuse UA Protein strip Renal 4+ Nonrenal +/- pos/neg pos/neg UA RBCs many occasional occasional UA Casts Renal: RBC Nonrenal: none Hemoglobin Myoglobin Bilirubin • The heme released from red cells is converted to the yellow bile pigment biliribin by a series of complex reactions in liver. A small amount is excreted under normal circumstances and is not detected in the urine with the dipstick. • When present, the Diazo Reaction is based on the coupling of bilirubin with a diazonium salt in an acid medium to form a colored azo-dye complex. Ictotest for Bilirubin • Highly pigmented urines can cause false positive reactions. Confirmation is required by testing with the Ictotest tablet test for bilirubin. • This diazo tablet method is very sensitive to low levels of bilirubin. • Pigments will be removed by the absorbent pad supplied with the test. CLINICAL SIGNIFICANCE BILIRUBIN • Reference value – not detected with reagent strips <0.02 mg/dL • Positive findings – obstruction to bile flow from liver • – inflammation and swelling of liver cells • • – gallstones and neoplasms of pancreas acute viral hepatitis, drug indued cholestatsis acute alcoholic hepatits/cirrhosis congenital hyperbilirubinemias • Dublin-Johnson and Rotor Urobilinogen • Collectively referred to as the end products of bilirubin metabolism. Colorless reduction product of bilirubin which is oxidized by normal intestinal bacteria to brown pigment that is excreted in the feces. • Based on the Ehrlich Reaction in an acid medium to form a red color. CLINICAL SIGNIFICANCE UROBILINOGEN • Reference value – – – – up to 1 mg/dL or 1 Ehrlich Unit greater in PM (alkaline tide after meals) up to 2 mg/dL transition from normal to abnormal decrease or absence cannot be determined with strip • Increased values – – – – liver damage: viral hepatitis, cirrhosis, drugs, toxins infections of biliary tree (cholangitis) hemolytic anemias and intravascular hemolysis increased enteric production • Absent – – obstruction of bile duct absence of intestinal flora UA BILIRUBIN & UROBILINOGEN in UNCOMPLICATED JAUNDICE Condition Bilirubin Urobilinogen Normal Hepatic Disease Obstructive Disease Hemolytic Disease Negative Positive Positive (+/-) Negative up to 2 EU/dL Increased (+/-) Absent Increased QUALITY ASSURANCE • Facilities and Resources – OSHA compliance • Proficiency Testing • Personnel – – Qualifications, education and training, competency Review • Procedure Manual – NCCLS GP2-A2 • Controls, Standards, Reagents • Equipment and Instruments • Reporting of Results COMPETENCY ALERTS REAGENT STRIP TESTING • Directly Observe – Followed SOP and manufacturer’s instruction • labeled date received, opened, expired • Removed strip immediately before test run • Replaced cap – – – – – – Performed test on well mixed, unspun urine Performed daily maintenance/function checks Interpretation of color changes for strips or tablets Performed confirmatory testing as indicated Performed Clinitest on nursery or pediatric urines Followed SOP step-by-step COMPETENCY ALERTS (continued) • Monitor and Review – Compliance with QC as defined in SOP • • • Results logged on scheduled frequency of use Parallel testing PM and service logs signed – Critical values reported on interim worksheets: WHO, WHAT, WHEN. – Standard units of measure defined in SOP are used to report qualitative and quantitative results. COMPETENCY ALERTS (continued) • Assessment of Test Performance – – Proficiency testing Internal blind samples of known chemical concentration • Problem Solving – – – – Resolve discrepant results Investigate and resolve delta checked results Specimen referred for definitive testing (UA culture) based on reagent strip results. Policy defined in SOP. Resolution of “out-of-control” results for known reference controls. MICROSCOPIC EXAM of URINARY SEDIMENT • CLIA’88 Complexity – – Moderate Provider Performed Microscopy (PPM) • • physician, midlevel practitioner, or dentist brightfield or phase microscopy • Specimen of Choice – – – – Fresh first morning, midstream, clean catch Examine within 2 hours Specific gravity >1.010 pH acid IDENTIFIABLE SEDIMENT ENTITIES • Hematopoietic cells – Red blood cells (RBC) • – dysmorphic white blood cells (WBC) • • • glitter eosinophils lymphocytes , histiocytes and macrophages • Epithelial cells – – – Transitional (urothelial) Squamous Renal tubular • oval fat bodies • Casts – – – – – Matrix : Hyaline and Waxy Cellular: RBC, WBC, Epithelial, Mixed, Bacteria Inclusion: Granular, Fatty, Hemosiderin, Crystal Pigment: Hemoglobin, Myoglobin, Bilirubin Size: Broad or Wide • Crystals • Microorganisms – bacteria, yeasts, parasites • Miscellaneous – spermatozoa, mucus, artifacts and contaminants