Acute Kidney Injury
advertisement
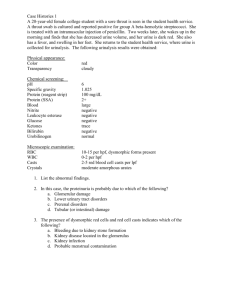
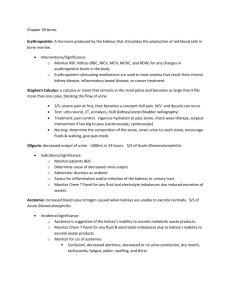
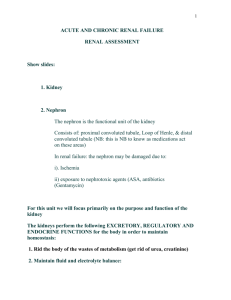
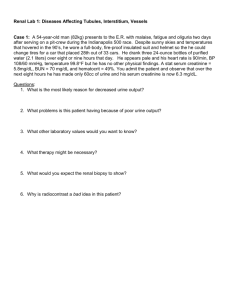
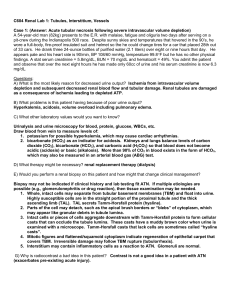
Acute Kidney Injury 49 year old man was a single vehicle MVC in which he was ejected. His injuries include: Left temporal epidural hematoma Left hemo/pneumothorax Liver laceration Bilateral open compound femur fractures He is brought to the ICU postop after an urgent craniotomy for the epidural. A chest tube is in place but the fractures are only splinted. 6 hours after admission, the nurse calls because the urine output has fallen. On assessment, he is sedated and intubated with both legs in traction. He is hemodynamically stable, BP 168/86, pulse 96, no vasopressors and afebrile. There is about 200 mL of dark urine in the foley bag (emptied upon arrival to ICU). Is there a problem with the urine output? The patient weighs about 75 kg and is known to have some renal insufficiency with a baseline creatinine of 200. Creatinine on admission was 305. Is there a problem with the urine output? RIFLE Criteria Risk Injury 3X increase in creatinine or UO < 0.5 ml/kg for 24 hours or anuria for 12 hours Loss 2X increase in creatinine or UO < 0.5 ml/kg for 12 hours Failure 1.5X increase in creatinine or UO < 0.5 ml/kg for 6 hours Complete loss of function for more than 4 weeks ESRD Complete loss of function for more than 3 months Where is the patient in the RIFLE criteria? List some possible causes for the renal dysfunction in this case. Volume depletion Radiocontrast dye Myoglobinuria Acute on chronic renal insufficiency Categorize the different causes of acute renal insufficiency. Prerenal: volume depletion and relative hypotension Vascular: Consider vasculitis, TTP, nephrosclerosis, renal artery stenosis Glomerular: Consider the nephritic and nephrotic syndromes Tubular/interstitial: Consider ATN, drugs, PCKD, myeloma, autoimmune disorders Obstructive: Consider prostate disease, stones, metastatic cancer What are the most likely causes in hospitalized patients? ATN (45%) Prerenal (21%) Acute on chronic kidney disease (13%) Obstruction (10%) Glomerulonephritis or vasculitis (4%) Acute interstitial nephritis (2%) Atheroemboli (1%) 6 hours later, the patient’s urine output has been a total of 350 mL since admission. The creatinine has risen to 455. What RIFLE criteria is the patient now? What investigations could be ordered to identify the cause of the acute kidney injury? What are the implications on morbidity and mortality when renal failure occurs in the ICU? The urine sodium is 125 mmol/L, urine osmolarity is 247 mOsm/L, serum osmolality is 315 mOsm/L, CK 98035, and urine myoglobin 15035. It is now 24 hours since admission and there has only been another 100 mL of urine with no urine for the last 12 hours. What is the RIFLE criteria now? What treatments could have been started to mitigate the development of acute kidney failure? What are the indications for renal replacement therapy in the critical care setting? How do you choose between continuous versus intermittent hemodialysis? After inserting a femoral dialysis catheter, the patient is started on hemodialysis. He is currently has a MAP of 65 requiring levophed 12 ug/min with a FiO2 of 85% (increased since starting fluid boluses. Will this patient tolerate an intermittent run of dialysis? Why or why not? How does hemodialysis work? What are the different modes of continuous renal replacement? Questions??