Urinary System Diseases
advertisement
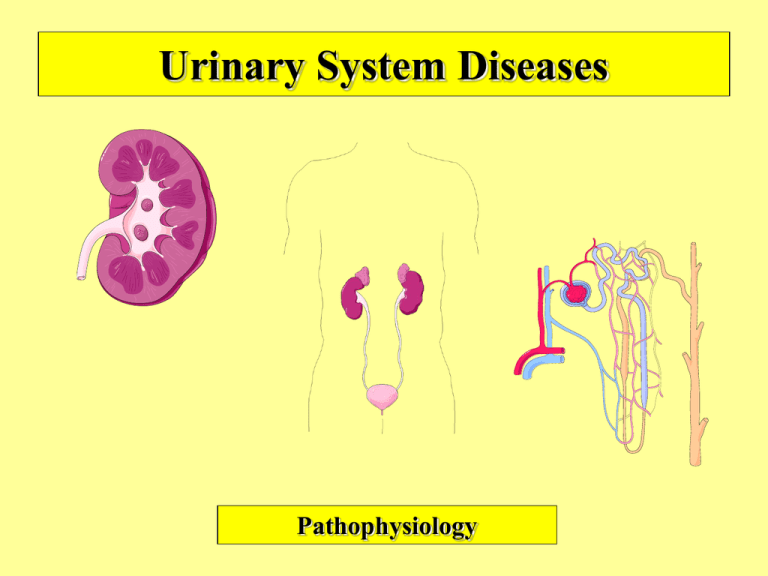
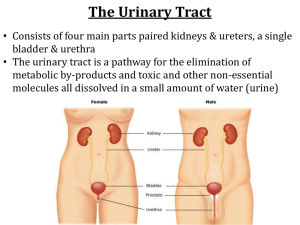
Urinary System Diseases Pathophysiology Review of Urinary Anatomy & Physiology • Located: – Under back muscles – Behind peritoneum • Thus: retroperitoneal – Below level of lowest ribs – Right lower than left – Adrenal gland on top of kidney • Cortex • Medulla – Contains Pyramids & Papilla • Pelvis – Calyx = division of pelvis • Pleural = calyces • Bladder – Lined with transitional epithelium • Can stretch – Lined with rugae – Trigone • On posterior wall • Where ureters & urethra open • Rigid area with NO rugae – Micturition (voiding, urination) • Internal urinary sphincter – Involuntary • External urinary sphincter – Voluntary • Stretch receptors in bladder wall • Nephron = functional unit – Consists of: • Renal Corpuscle • Renal Tubules • Renal Corpuscle contains: – Bowman’s capsule • Part of collecting system – Glomerulus • Afferent arteriole • Efferent arteriole • Renal Tubules 1. Proximal convoluted tubule 2. Loop of Henle 3. Distal convoluted tubule 4. Collecting tubule • Key point: – The cortex contains all the structures of the nephron – The medulla contains only the collecting ducts & the loop of Henle • Functions of the kidney 1. Removes nitrogenous wastes – – – – 2. 1. 2. – – 3. – Juxtaglomerular apparatus RAA system » Renin » Angiotensin » Aldosterone – 4. Occurs in proximal convoluted tubule Also occurs in distal convoluted tubule It takes things back into blood Secretion – Via blood filtration & formation of urine Occurs in renal corpuscle Reabsorption – Regulation of Blood Pressure – Filtration – Fluid balance Electrolyte balance Acid-base balance Excretory Organ – 4. Urine formation Maintains homeostasis – – – 3. Urea Uric acid Creatinine Ammonia • Occurs in distal convoluted tubule Blood gives things up to the urine Concentration – Occurs in collecting tubules See next slide Some Key Points of Renal Physiology • Nitrogenous wastes primarily come from breakdown of proteins • Aging & renal function • By age 35, one begins to lose nephrons • By age 80, one has approx. 30% reduction in nephron capacity • GFR = glomerular filtration rate – Normal = 125cc/min (7500cc/hour) – 99% of filtered product is reabsorbed » Normal urine output = 60cc/hour (1500cc/day) • All along the duct system water is reabsorbed – Includes the prox. conv. tubule, loop of Henle, distal conv. Tubule, & collecting tubule – Sodium follows water • Key elements involved in each process – Reabsorption = H2O(Na), proteins (amino acids), & sugars (glucose) – Secretion = ions(K+), drugs, ammonia – Concentration = more reabsorption of H2O • 2 key factors determine volume of urine produces 1. Glomerular filtration rate (GFR) – Determined by the unique arrangment of blood vessels 2. Hormonal secretion – Determined by fluid & electrolyte balance Volume of urine also controlled by glomerular filtration rate • • • Unique arrangment of blood vessels – Afferent arteriole -----to----capillary bed-----to----efferent arteriole -----to----capillary bed ----to---- veins • First capillary bed = glomerular capillaries • Second capillary bed = peritubular capillaries Purpose of this = to control the pressure in the glomerular capillaries & consequently the glomerular filtration pressure 3 factors control this: • (1) autoregulation • Local feedback from muscle tension in afferent arteriole • Local feedback from DCT at JGA • Mediated via endothelial secretions of glomerular capillaries • (2) sympathetic nervous system • (3) renin • • • B = increase fluid volume; overhydration; high output heart failure C = kidney pathology D = hypertension; arteriolar spasm – Hormones help control the volume of urine via fluid & electrolyte balance • The concentration factor essentially deals with urine volume – Usually more the volume = more the dilution [a direct proportion] 1. Aldosterone » From adrenal cortex » Works on distal convoluted tubule » Causes H2O & Na+ retention 2. Atrial natriuretic hormone(ANH) » » » » From atrial wall of heart Works on distal convoluted tubule Works in opposition to aldosterone Causes H2O & Na+ loss 3. Antidiuretic hormone » From posterior pituitary » Works on collecting tubules » Causes reabsorption of H2O (Na+ goes with it) Diagnostic Tests - Urinalysis 1. Physical Characteristics & Measurements – appearance – color – odor – volume – specific gravity 2. Chemical Measurements – pH – protein; glucose – ketones – bilirubin; urobilinogen – leukocytes; nitrite – blood 3. Microscopic – cells (wbc, rbc, sperm) – casts – crystals – bacteria 4. Detection of Bacteriuria – nitrite test • qualitative or screening test – C&S • Colony Count, if done, make this a quantitative test • NOTE: Step 4, qualitatively, is done as part of step 2 • Appearance – – – – Clear = normal Cloudy = ? Infection If sediment = kidney disease Dark = ?blood, ?bilirubin, ?concentrated • Color – Urochrome pigment = yellow • comes from breakdown of hemoglobin – Concentration • More Concentrated = Deeper Yellow – Change of Color From: • Meds – Vitamin = yellow • Diseases – Blood = red-brown – Liver = Orange • Foods – Rhubarb = red-brown • Odor – Normal = ammonia-like smell • from breakdown of urea – Unpleasant = ? infection • Quantity – Average per 24 hours = 1500 cc • 60 cc per hour • GFR = 125 cc/min – Thus, 7500 cc/ hour • Urine Made Per Hour = 60 cc • Urine GFR Per Hour = 7500 cc – KEY: 1 % of filtered urine remains urine; 99 % becomes reabsorbed back into blood – Oliguria = 100 - 400 cc per day – Anuria = less than 100 cc per day – Polyuria = diabetes, nerves, diuretics • Specific Gravity – – – – – Determines Concentration Compares Test Liquid to H2O Normal = 1010 - 1030 First AM Specimen = > 1020 In many kidney diseases, one loses the ability to concentrate urine – 3 ways to do it: 1. Reagent Strip 2. Refractometer 3. Urinometer • pH – Determines Acidity or Alkalinity – Normal = 6.0 – Range = 4.5 - 8.0 • Acidity example = diabetes • Alkaline example = UTI • Protein – OK to have a Trace in the urine – Benign Conditions: • exercise • exposure to cold • protein consumption – Generally Means Kidney Disease • Glucose – Will only be in urine if exceed Renal Threshold (160 - 180 mg/dl) • Ketone (note Acetone is a Ketone) – Ketones are products of Fat Metabolism – If cant breakdown Sugars for energy, the body will begin using Fat – Seen in: • Uncontrolled Diabetes • Starvation • Hi-Fat Diet • Bilirubin & Urobilinogen Formation – When used-up RBC’s are broken down by R-E System, a by-product is Bilirubin – Bilirubin removed from blood by liver & excreted into intestine – Bacteria in intestine convert Bilirubin into Urobilinogen – Some Urobilinogen reabsorbed into blood • Of this amount reabsorbed some my be normally passed in urine • Bilirubin – Normally None in Urine – Found in urine if it can’t get from the liver into G-I tract • From Obstruction of Bile Ducts – Found in urine if have: • Liver Disease (hepatitis) • Blood Disease (hemolysis) • Urobilinogen – generally follows whatever happens to bilirubin – may get none in urine if on antibiotics (destruction of gut flora) – usually get small amount in urine • Blood – None is normal – But may see some if female is menstruating • Leukocytes – from inflammation of kidney or lower G-U tract • Nitrites – screening test for bacteriuria – bacteria convert nitrate to nitrite Other Diagnostic Tests • Blood tests • • • • BUN / creatinine CBC ------ anemia if decreased EPO production Renin Antistreptolysin titers • Urine culture & sensitivity (C&S) • Include colony count • Imaging • IVP • Retrograde pyelography • CAT/ MRI • Surgical procedures • Cystoscopy • Biopsy Urinary Tract Disorders overall outline • • • • • Incontinence & retention UTI’s Inflammatory disorders Nephrotic syndrome Urinary tract obstruction • Stones • Hydronephrosis • Tumors – Renal cell carcinoma – Bladder cancer • Congenital disorders • Polycystic kidneys • Wilm’s tumor (nephroblastoma) • Renal failure • Acute • Chronic • Dialysis Incontinence, retention, & catheters • Urinary Incontinence – – – – – Loss of voluntary control of bladder Frequently called “neurogenic bladder” Many causes Enuresis = involuntary control after age 4 or 5 Types: – Stress – Urge – Overflow • Urinary retention – Called “residual urine” – Causes : – Anatomical defects – Neurogenic defects • Treated with “catheterization” – Foley – French Urinary Tract Infections Urethritis; Cystitis; Pyelonephritis • • • • Etiology – Ascending infection ----- women > men – Prostatic hypertrophy with urinary retention – Incomplete emptying of bladder with urinary stasis – Pregnancy associated with stasis – Blood borne pathogens Pathophysiology of UTI’s ----- see next slide Dx • Dysuria, urgency, & nocturia • Systemically get fever & malaise • CVA tenderness in pyelonephritis Note glomerulonephritis is vastly different with regards etiology & pathophysiology • Note etiologies – Inflammation of mucosa – Trauma of mucosa – Obstruction – Vesicoureteral reflux – Immobility – Blood-borne pathogens • TB • HIV • Septicemia Inflammatory disorders (1) glomerulonephritis (2) nephrotic syndrome • Glomerulonephritis – Acute • Sx = proteinuria, edema, oliguria • Etiol = 1-2 weeks post strept infect. – Chronic • Etiol = autoimmune disease – e.g. lupus, diabetes, hepatitis C • Can lead to irreversible kidney damage • Nephrotic Syndrome – Glomerular disorder where one loses the capacity to retain protein, especially albumin – Sx – severe edema (anasarca) * can get skin breakdown since impaired arterial flow – proteinuria – hypoalbuminemia – oliguria – Etiol: » Toxic agents (lead, mercury) » Toxic drugs (aminoglycosides) » Diseases (diabetes, lupus » Key = any significant problem with glomerulus can lead to nephrotic syndrome Obstructive Disorders • Renal Calculi – Etiology: Calcium, Uric acid, Urine crystals – Symptoms: renal colic, N&V, chills, fever – Risk factors: prolong dehydration, prolong immobilization, infection – Treatment: surgery,lithotripsy • Anomalies – – – – Strictures Kinks Ptosis Pelvic kidney • Tumors – Note that primary symptom = hematuria – Renal Cell Ca = most common, unilateral, adeno Ca from tubular epithelium • See picture – Bladder Ca = usually from transitional epithelium • Neurogenic bladder – • These result in: – Hydronephrosis – Hydroureter If these conditions exist longer than 2 months get destruction of kidney Major sites of urinary tract obstruction Congenital Diseases • Vesicoureteral reflux • Due to ectopic insertion of ureter into bladder. If far away from trigone, do not get adequate compression of ureter when voiding & get reflux • Incidence: 1/1000 • If one gets it each sibling(to be) has 50% incidence • Girls> boys; 10:1 ratio • Ectopic kidney • May get kinking of ureter • Usually in pelvis • Asymptomatic • Renal agenesis • • • • Usually unilateral & left kidney 2 types: (1) occurs randomly (2) genetic Asymptomatic Remaining kidney becomes large since compensatory hypertrophy Congenital Diseases (cont) • Polycystic kidney (2 types – In adults (see picture) • Genetic etiol ----- autosomal dominant • Clinically seen in adults – Between age 30 – 40 one begins to get renal failure • Tx = transplant – In children • Genetic etiol --- autosomal recessive • Manifest at birth; usually fatal or infant stillborn • Rare • Wilm’s tumor (nephroblastoma) • Most common tumor of children; usually unilateral • Etiol = autosomal recessive (on chromosome 11) • Manifests between age 2 – 5 years & presents as abdominal mass – May produce hypertension • 5 year survival = 90% Renal Failure • Acute renal failure – Abrupt decrease in renal function • Nitrogenous wastes accumulate – Usually reversible – Sx: • Oliguria • Drowsiness • Altered levels of consciousness – Etiol: • Glomerular disease • Severe pyelonephritis • Nephrotoxins that damages tubular epithelium • Ischemic causes – shock • ATN (acute tubular necrosis) » e.g. burns(hgb accumulates) » e.g. trauma (myoglobin accumulates) • Chronic Renal Failure – Get slow progressive loss of neurons – Usually irreversible – Course = gradual – Etiol: • Vascular disease – e.g. hypertension – Disease called nephrosclerosis • Glomerular disease – e.g. diabetes • Tubular disease – e.g. toxins Hypertension & the kidneys Dialysis in renal failure • • 2 types: – Hemodialysis – Peritoneal dialysis Mechanism – Simple diffusion for wastes & electrolytes – Osmosis for water balance