Hyperkalemia – a renal emergency?
advertisement

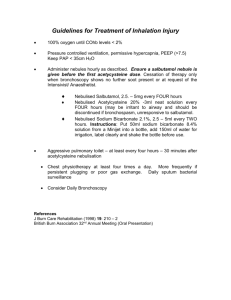
Hyperkalemia – an emergency? Shaila Sukthankar Paediatric Nephrology Study Day 22.06.12 RMCH Hyperkalemia Overview Clinical cases Emergency Management Hyperkalemia - causes Spurious/ pseudohyperkalemia Increased intake Trans-cellular shift Decreased renal tubular excretion – Renal – Endocrine – Drugs Investigations Renal – U&Es, acid base balance, urinalysis – TTKG (urine K X P osmol/ plasma K X U osmol) Endocrine – For another meeting! – Renin, aldosterone, urinary steroids, 17-OHP Others – FBC, blood film, urate, CK, calcium, phosphate Case 1 ER, 15 years old girl Known to have IDDM for several years Difficult family circumstances but ER very well engaged and compliant Recent annual diabetes review 3 months before admission - good glycaemic control Blood tests unremarkable, urine microalbumin/ creatinine ratio normal Growth – weight and height 2nd to 9th and postpubertal Clinical Presentation Diarrhoeal illness for 1 week – mucus, no blood. Initially polyuric and nocturic, now decreased urine output Parents noticed her to be pale and tired lately Examination – pale, BP 130/ 86, hydration and perfusion normal Urine 3+ glucose, ketones ++ Initial investigations CBG: pH 7.2, BE –10, Bicarb 15 Na 128, K 6.5, urea 23 Hb 9.8, WCC 5.8 Further investigations Platelet 240 Glucose 7.8 Creatinine 210 Ca 1.9, Pi 2.8 Blood film – normal RBC and platelet morphology Urine 2+ protein, 3+ blood with casts Immediate measures Stop external sources of K Stabilise myocardium – IV calcium gluconate Enhance intracellular shift of K – Nebulised Salbutamol – Sodium Bicarbonate – Glucose Insulin infusion Increase excretion – Ion exchange resin – Dialysis Calcium Gluconate If K >7 mmol/ L or ECG changes 10% solution 0.5 ml/ Kg (maximum 20ml) over 10 minutes With ECG control via large peripheral or central line Protects myocardium from acute dysrhythmia, no effect on K levels Salbutamol First line treatment – nebulised 2.5mg up to 5 years age, 5mg there after Can be repeated up to 3 times Alternatively, if access available, IV salbutamol – – – – 4mcg/ kg diluted with normal saline or glucose 50mcg/ml concentration Over 5 min as slow bolus Does not lower net K, shifts from ECF to ICF Sodium Bicarbonate In presence of acidosis 8.4% solution 1ml (1mmol)/ Kg Diluted to minimum 1:10 with normal saline/ glucose for peripheral venous use (1:5 for central access) Infusion over 30 minutes Shifts K from ECF to ICF Glucose Insulin infusion Soluble short acting insulin (0.1 U/ Kg) Mixed in 5 – 10 ml/ Kg of 10% dextrose for peripheral use (2.5 to 5 ml of 20% dextrose for central access) Infused over 30 minutes Check BM every 15 minutes by POCT – until 15 minutes after infusion Calcium Resonium Oral (not neonates) or rectal 125-250 mg/ kg qds (maximum 15gm per dose) If given orally, also use lactulose Lowers total body K by excretion in stools Further management Treatment of underlying cause – DKA management, endocrine, renal etc Renal replacement modalities – Haemodialysis for rapid effective reduction in K levels – Peritoneal dialysis is as effective but over longer duration – Haemofiltration – if already on ICU After emergency treatment… Recheck U&Es after 15 minutes of initial intervention to ensure – treatment is effective – Level is reaching safe range Recheck after 1 – 2 hours to detect rebound hyperkalemia Look for underlying cause ER - update Required nebulised salbutamol and Ca gluconate at local DGH Transferred to RMCH and started on dialysis the same day Had immune work up and renal biopsy GFR reduced to <10 (ESRD) – CKD5 management On dialysis Had living related donor kidney transplant Case 2 3 years, boy, previously well Presented with fever and frequent URI Growth, examination normal Blood tests – – – – FBC normal, mild iron deficiency Na 135, K 6.8, U 4.5, Creatinine 35 pH 7.3 BE – 8, sugar 4.8, urine NAD ECG nSR Case 2 continues… Plasma renin and aldosterone low Synacthen test and 17-OHP normal Diagnosis?? – Hyporeninemic hypoaldosteronism – Pseudohypoaldosteronism Gordon’s syndrome (PHA 2) Tubulopathy affecting chloride channels, decreased potassium excretion (WNK1, WNK4 AR mutation) Responded well to thiazide diuretics Younger twin siblings also affected All currently well with normal K levels on thiazide treatment Summary Acute, severe, true hyperkalemia – is a medical emergency – requires prompt recognition and optimum treatment Not all hyperkalemia is renal in origin Specialist input required to establish etiology and long term management Specialist Input Assessment Action Abnormal renal function D/w Nephrology Massive hemolysis/ rhabdomyolysis or tumor lysis Normal renal function D/w Nephrology (+ hemato-oncology) Uncertain D/w All D/w Endocrinology (+/nephrology)