What are values and preferences?
advertisement

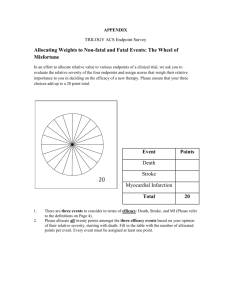
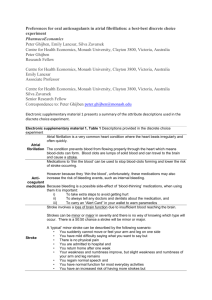
Gordon Guyatt Clarity Research Group McMaster University what is the problem? whose values and preferences? how can we find out about values and preferences? applying best estimates of V and P almost all decisions/recommendations involve tradeoffs benefits versus harms, burden, costs antithrombotic therapy thrombosis reduction vs bleeding, burden, costs tradeoffs require V and P judgments value reducing MI, stroke, DVT vs bleed and burden guideline panel members health care providers policy makers subjects of the guideline patients general public systematic review of patient V and P use guideline panel members act as proxies for their patients’ V and P patients on panel collect own values and preferences data comprehensive search 48 studies 16 a fib, 10 stroke or MI, 5 VTE, 17 burden higher disutility on stroke than gastrointestinal bleed and much greater disutility on stroke than on treatment burden example of the relative value of health states: a reasonable trade-off between nonfatal stroke and bleeds is a ratio of disutility of 2.1 to 3.1 systematic review results require interpretation how should guideline panel proceed? systematic V and P rating exercise ACCP consider systematic review make ratings for typical patients rate scenarios, time frame of one year Full Health Maximum Feeling thermometer: Venous limb gangrene Mean Minimum Dead 13 Physical Symptoms Mental Symptoms Pain Recovery Further Risk Your child suddenly becomes unresponsive Your child is unable to move one arm and one leg Your child cannot speak to you Your child is irritable and upset You find it difficult to console your child Family and friends find the diagnosis difficult to accept Your child has a headache for a number of days Your child’s stay in hospital is prolonged Your child recovers some function, including speech and movement slowly over weeks to months Your child complains of tiredness for months Your child needs help to attend normal school Your child has multiple hospital visits for physiotherapy and rehabilitation You must alter your hopes and dreams for your child’s future You are told your child is not at risk of further strokes, You find your child’s ongoing limitations very hard to accept 14 Full Health Maximum Feeling thermometer: Major stroke in a child Mean Minimum Dead 15 Symptoms Diagnostic tests and treatment Recovery You feel nauseated and unwell for two days, and then suddenly you vomit blood and feel faint. You are taken by ambulance to a busy emergency department. An intravenous catheter is placed and a catheter is placed through your nose into your stomach to help drain the blood You receive blood transfusions to replace the blood you lost You are admitted to hospital A doctor puts a tube down your throat into your stomach to see where you are bleeding from and to provide treatment You receive sedation by intravenous to ease the discomfort of the test You do not require an operation to stop the bleeding You must stop taking your blood thinner; stopping the blood thinner puts you at risk of developing a new blood clot. You stay in the hospital for a few days You feel much better at the end of your hospital stay You need to take pills for the next six month to prevent further bleeding After that, you are back to normal About 2 weeks after your bleeding you restart your blood thinning therapy – you worry every day about more bleeding for the first month after restarting After that, your worry gradually decreases 16 Full Health Maximum Feeling thermometer: Gastrointestinal bleed Mean Minimum Dead 17 myocardial infarction = pulmonary embolus = venous thrombosis = gastrointestinal bleed stroke = 3 bleeds (and thus three of any other major event) strong recommendation confident more good than harm almost all informed patient make same choice tight balance uncertainty about typical V and P uncertainty about variability in V and P V and P highly variable Strong recommendation for warfarin often advocated may be useful in issues overlooked no guarantee reflects typical V and P establish that everyone agrees with evidence summary clarify values and preferences Review evidence about patient V and P value and preference judgments ubiquitous panels MUST make judgments explicit quantitation desirable values those who bear consequences weak recommendation more likely close trade-off uncertainty in typical V and P highly variable V and P systematic review of V and P – routine still need panel input study results require interpretation results likely incomplete structured elicitation of panel V and P patients on panel – questionable expert panel shared decision-making