Pophyria
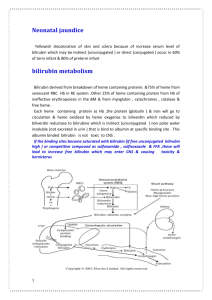
advertisement

Heme Metabolism •Heme biosynthesis and Porphyrias •Heme degradation: Jaundice Heme Biosynthesis: Porphyrias • Cruelly referred to as a Vampire’s disease. Thought to be a cause of the madness of King George III. • Can be caused by lead poisoning: The fall of the Roman Empire! Not a ‘vampire’s’ disease Some symptoms of porphyrias have lead people to believe that these diseases provide some basis for vampire legends: Extreme sensitivity to sunlight Anemia This idea has been discarded both for scientific reasons: Porphyrias do not cause a craving for blood. Drinking blood would not help a victim of porphyria. And for compasionate reasons:Porphyria is a rare, but frightening condition: hard to diagnose and there is no cure. The Madness of Inbreeding George III : Severe abdominal pain, mental confusion, dark urine. Mitochondria GLYCINE + SuccinylCoA d-aminolevulinic acid(ALA) Porphobilinogen(PBG) hydroxymethylbilane uroporphyrinogen III coprophyrinogene III Protoporphyrinogene IX protoporphyrin IX Heme PORPHYRIAS Agent Orange ALA synthase 3p21/Xp11.21 ALA dehydratase ALA-dehydratase Deficiency porphyria PBG deaminase Acute intermittent porphyria Uroporphyrinogen III cosynthase 10q26 Congenital erythropoietic porphyria Uroporphyrinogen decarboxylase Prophyria cutanea tarda Coproporphyrinogen oxidase 9 Herediatary coproporphyria Protoporphyrinogen oxidase 1q14 Variegate porphyria Ferrochelatase Erythropoietic protoporphyria 9q34 11q23 1q34 18q21.3 COORDINATED REGULATION OF HEME AND GLOBIN SYNTHESIS: Heme: inhibits activity of pre-existing d-ALA synthase diminishes the transport of d-ALA synthase from cytoplasm to mitochondria after synthesis of the enzyme. represses the production of d-ALA synthase by regulating gene transcription. stimulates globin synthesis to ensure that levels of free heme remain low in concentration. Inhibition of the synthase and stimulation of globin synthesis are the most important aspects in balancing hemoglobin production. Heme Degradation NADPH HEME O2 NADP+ Fe+3 (opens the porphyrin ring) BILIVERDIN NADPH NADP+ BILIRUBIN BILIRUBIN diglucuronide BILE Heme Catabolism Jaundice Hyperbilirubinemia: Two forms: Direct bilirubin: Conjugated with glucoronic acid Indirect bilirubin: unconjugated, insoluble in water. What’s the cause of jaundice? 1- Increased production of bilirubin by hemolysis or blood disease: •Increase in blood indirect bilirubin •Called pre-hepatic jaundice •Stool color remains normal. 2- Abnormal uptake or conjugation of bilirubin: •Leads to non-hemolytic unconjugated hyperbilirubinemia •Increased indirect bilirubin. •Stool color turns gray. •Caused by liver damage or disease. What’s the cause of jaundice? 3- Cholestasis = Problems with bile flow. a: Intrahepatic cholestasis: hyper conjugated bilirubinemia •Increase in blood indirect and direct bilirubin •Caused by liver damage or disease: eg cirrhosis, hepatitis •Can also occur in pregnancy: b:Extrahepatic cholestasis: •Blockage of bilirubin transport in the bilary tract. •Increased direct bilirubin. •Stool color turns gray. •Caused by: Tumors or gall stones. CLINICAL PREMISE Newborns often have a yellowish tint to their skin. This condition is known as jaundice and results from the infant ridding itself of "fetal" hemoglobin which will be replaced by "adult" hemoglobin. As you will learn in this lecture, catabolic products from hemoglobin are removed by the liver. However, the infant's liver is often too immature to handle the excessive breakdown products. Instead they accumulate giving the yellowish tint. Exposure to mild UV light from the sun is usually sufficient to destroy these compounds, although in very severe cases blood dialysis may become necessary as these byproducts can be toxic. Table 1- The porphyrias. You are responsible for the enzyme defects in red Type Enzyme Involved Major Symptoms Acute intermittent porphyria Uroporphyrinogen synthase Abdominal pain Neuropsychiatric urinary porphobilinogen Congenital erythropoietic porphyria Uroporphyrinogen cosynthase Photosensitivity urinary uroporphyrin Porphyria cutanea tarda Decarboxylase Photosensitivity Variegate porphyria Oxidase Erythropoietic protoporphyria Laboratory tests porphobilinogen urinary uroporphyrin porphobilinogen Ferrochelatase Photosensitivity Abdominal pain Neuropsychiatric urinary uroporphyrin fecal coproporphyrin fecal protoporphyrin Photosensitivity fecal protoporphyrin red cell protoporphyrin BLOOD CELLS Stercobilin excreted in feces Urobilin excreted in urine Hemoglobin Globin Heme O2 Heme oxygenase Urobilinogen formed by bacteria INTESTINE KIDNEY reabsorbed into blood CO Biliverdin IX via bile duct to intestines NADPH Bilirubin diglucuronide (water-soluble) Biliverdin reductase NADP+ Bilirubin (water-insoluble) 2 UDP-glucuronic acid via blood to the liver Bilirubin (water-insoluble) LIVER Figure 2. Catabolism of hemoglobin Figure 3. Examples of hyperbilirubinemia A. Hemolytic anemia B. Hepatitis C. Biliary duct stone excess hemolysis unconjugated bilirubin (in blood) conjugated bilirubin (released to bile duct) unconjugated bilirubin (in blood) conjugated bilirubin (in blood) unconjugated bilirubin (in blood) conjugated bilirubin (in blood) Table 2- Genetic Disorders of Bilirubin Metabolism Condition Defect Bilirubin Clinical Findings Crigler-Najjar syndrome severely defective Unconjugated UDP-glucuronyltransferase bilirubin Profound jaundice Gilberts syndrome reduced activity of Unconjugated UDP-glucuronyltransferase bilirubin Very mild jaundice during illnesses DubinJohnson syndrome abnormal transport of conjugated bilirubin into the biliary system Moderate jaundice Conjugated bilirubin Formation of porphobilinogen: Lead Poisoning Cyclization to the porphyrin Cyclization to the porphyrin