Clinical Cases
advertisement
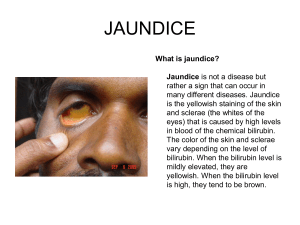
Clinical Cases Dr. Faller – Sickle Cell Anemia I. II. III. IV. PRESENTATION a. Around 6-7 months b. Symptoms: i. Rapid breathing, heart rate, murmur ii. Enlarged spleen iii. Dactylitis (enlarged hands and feet) c. To diagnose: take blood sample, remove O2, see if there is sickling GENETICS/BIOCHEMISTRY a. 1 copy of gene – protects from malaria (sickle cell endemic wherever malaria present) b. 2 copies of gene – disease: i. Single base mutatation - 6 Glu becomes Val ii. Patients have 22 and 2S2 PATHOPHYSIOLOGY a. Tetramers aggregate and form elongated tubes b. Polymerization occurs when Hb in deoxy form - changes shape of cell to sickle shape c. Cell can reoxygenate and revert back to normal shape for a few cycles, but after a while too much membrane damage – can no longer oxidize – starts to deform d. Components of disease: i. Vasoocclusion: sickle cells can get through vessel and build up (also build up in other structures) ii. RBCs finally burst (hemolysis) after sickling and release chemicals 1. nitric oxide – changes in vessel tone –affects ability to relax 2. damage to endothelial tissues e. Sickling enhanced by i. Hypoxia – decreases O2 availability ii. Stasis – increases o2 extraction in tissues iii. RBCs release more O2 (disease propagates itself) THERAPIES a. Pain medication (morphine), hydration, oxygen (never been shown it actually helps) b. Try to relieve dactylitis c. Prophylactic antibiotics – to replace spleen’s job of clearing bacterial infections i. Daily penicillin ii. Vaccines – but not good response without spleen iii. Rapid cultures and treatment for infections d. Folic acid – RBCs unstable and break down – require folic acid to make new ones e. Hydroxyurea – chemo drug f. *α-amino butyric acid (first observed in patients with diabetic mothers) transcriptionally reactivates fetal hemoglobin – only need about 20% fetal Hb to ameliorate all complications – any amount to extend life span Dr. Nunes – Bilirubin Metabolism I. II. III. BILIRUBIN METABOLISM – see Offner notes HYPERBILIRUBINEMIAS a. Pre-hepatic – increased BR production – doesn’t have to do with liver i. Hemolysis (incr RBC destruction) – increased production of BR 1. excess unconjugated BR 2. no BR in urine 3. increased urobilinogen (if BR makes it to liver is conjugated normally) ii. ineffective erythropoesis b. Hepatic – metabolic abnormalities i. Problems with conjugation (Gilbert’s, Crigler-Najjar): 1. normal BR production but failure to conjugate increased unconj BR in blood(poss. jaundice) 2. no increase in urobilinogen 3. no BR in urine ii. Other causes of poor conjugation 1. Hepatitis – due to direct hepatic injury – viral or autoimmune 2. Drug-induced causes of liver injury 3. Cirrhosis – liver failure c. Post-hepatic i. Obstruction of bile flow: gallstones, structure of bile duct, pancreatic cancer, bile duct cancer, surgical injury ii. Normal production of BR, but can’t be excreted: 1. conj BR found in blood 2. incr BR excretion by kidneys (BR in blood - dark urine), 3. pale stools (no BR in stool) DIAGNOSING TYPE OF HYPERBILIRUBINEMIA a. Levels of BR in blood i. Excess unconjugated BR – prehepatic (just more BR) or hepatic (can’t conjugate) ii. Conjugated BR – posthepatic (can’t excrete via bile duct, intestines) b. Leves in urine/stools i. High urobilinogen – prehepatic (more BR being processed) ii. No urobilinogen - posthepatic iii. Dark urine =conj BR in blood – due to hepatic or post-hepatic iv. Pale stools – post-hepatic c. Levels of enzymes i. AST (cytoplasmic and mitochondrial enzyme, found in many organs) and ALT (cytoplasmic enzyme, more specific to liver) found in hepatocytes; when liver injured these enzymes can be released back into blood ii. Alkaline Phosphatase, GGT - enzymes associated with transport and excretion of BR into bile – obstruction often results in increase in levels of these enzymes Dr. Lowe, Dr. Offner – Sporadic Porphyrias I. II. III. RISK FACTOR – HEPATITIS C a. Much more common than Porphyria, mostly asymptomatic b. Causes: injection drug use, transfusions before 1992, dialysis, immigration, sexual transmission(<1%), clotting factor before1987 c. Progression of disease i. Acute Hep C – often leads to chronic Hep C, but only fraction get sick ii. Cirrhosis – then chance of liver failure or hepatocellular carcinoma d. Pathology of Cirrhosis i. Scarring in liver – fibrous bands replace healthy hepatocytes ii. Hepatocytes become hemmed in by fiber (blood supply gets cut off) = nodule iii. Treatment : weekly injections of pegylated interferon combined with antiviral – eliminated virus and liver can then heal (a liver transplant only “resets clock” iv. Alcohol is more likely to progress Hep C PORPHYRIA CUTANEA TARDA a. Pathophysiology: i. Due to uroporphyrinogen III decarboxylase deficiency ii. Uro’gen III builds up, oxidizes to porphyrin – deposited in various areas incl. skin b. Contributors: i. Photoreactive: skin damage occurs due to sun exposure, during warm months ii. Alcohol can result in porphyria cutanea tarda (if enzyme deficiency already present) iii. Iron overload c. Clinical features i. Bullous lesions (fluid-filled) on sun-exposed areas ii. Hypertrichosis (hair above beard line) iii. Urine turns pink under fluorescent lamp d. Therapy i. Treat Hep C ii. Avoid alcohol iii. Minimize sun exposure iv. Remove iron via phlebotomy VARIEGATE PORPHYRIA (RARE) a. Hundreds of single base mutations can cause deficiency in proto’gen IX dehydrogenase b. Acute attacks: neurological symptoms, skin symptoms, GI symptoms, photosensitivity c. Also called i. “South African Porphyria” (incidence can be as high as 3/1000) ii. “Royal Malady” (King George - periods of bizarre behavior, nausea, abdominal pain; due to stimulation from arsenic, thought to medicate) Learning Objectives Dr. Faller- Sickle Cell Anemia 1. Why the presentation of sickle cell anemia occurs around 6-7 months of age. 2. The role of protein aggregation and underlying biochemical/genetic basis for this in sickle cell anemia. 3. The pathophysiology of sickle cell anemia. 4. Why α-amino butyric acid is a successful therapy. Dr. Nunes – Bilirubin Metabolism 1. How bilirubin is metabolized and excreted in normal physiology 2. How hyperbilirubinemias can result from pre-hepatic, hepatic and post-hepatic causes as well as the biochemical basis for each of these disorders 3. How each type of hyperbilirubinemia results in a different clinical presentation which can be distinguished by evaluating levels of conjugated and unconjugated bilirubin in blood, levels of bilirubin and urobilinogen in urine and levels of the hepatic enzymes AST/ALT and alkaline phosphatase. Dr. Lowe – Porphyria 1. The enzyme defects leading to the porphyrias (from Offner)