Neonatal Jaundice SGD
advertisement
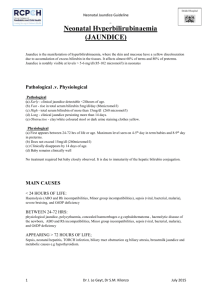
Neonatal Jaundice SGD Dr Saffiullah AP Paeds By the end of this discussion you should be able to; 1.Make a differential diagnosis of common and significant causes of jaundice in neonates 2.Differentiate between physiological and pathological jaundice including persistent jaundice in neonates 3.Organise investigations for neonates presenting with jaundice 4.Management of common and significant causes of neonatal jaundice 5.Indications and side effects of different treatment modalities of neonatal jaundice including phototherapy Learning outcomes ◦ Clinical jaundice appears at 2-3 days. ◦ Total bilirubin rises by less than 5 mg/dl per day. ◦ Peak bilirubin occurs at 3-5 days of age. Peak bilirubin concentration in Full-term infant <12mg/dl Peak bilirubin concentration in Premature infant <15mg/dl Physiologic jaundice ◦ Clinical jaundice is not resolved in 2 weeks in the term infant and in 4 weeks in the Preterm infant. ◦ Clinical jaundice appears again after it has been resolved. ◦ Direct(conjugated) bilirubin concentration is more than 1.5 mg/dl . Pathologic jaundice A 10 hours old baby boy born at term developed jaundice? 1.What 6 relevant things would you ask in the history? 2.What 6 relevant things would you look for in examination? 1.What 6 investigations you would order? 2.How would you plan the treatment? 3.What 2 treatment modalities would you consider? Case 1 SBR 20 mainly indirect Hb 10, wbc 8000 and platelets 300000 Mothers blood group O Rh positive, Baby’s A Rh positive Coombs test positive Case 2 SBR 20 mainly indirect Hb 10, wbc 8000 and platelets 300000 Mothers blood group B Rh negative, Baby’s A Rh positive Coombs test positive Case 3 SBR 20 mainly indirect Hb 10, wbc 8000 and platelets 300000 Mothers blood group A Rh positive, Baby’s A Rh positive Coombs test negative Blood film showed spherocytes Case 4 SBR 20 mainly indirect Hb 10, wbc 20000 and platelets 300000 Mothers blood group A Rh positive, Baby’s A Rh positive C reative protein CRP 150 Coombs test negative Case 5 SBR 20 mainly indirect Hb 10, wbc 8000 and platelets 300000 Mothers blood group A Rh positive, Baby’s A Rh positive Coombs test negative G6PD low Case 6 Multiple Single 550 Total serum bilirubin (micromol/litre) 500 Exchange transfusion 450 400 Phototherapy 350 300 250 200 150 100 50 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Days from birth Increased water loss Diarrhea Retinal damage Bronze baby, tanning Mutations in DNA? shield scrotum Disturb of mother-infant interaction Side effects of phototherapy 4 weeks old baby girl presented with jaundice which started in the first couple of days.On examination she was jaundice and has hepatomegaly. 1.What 6 important questions would you ask from her mother to help you with diagnosis? 2.What 4 investigations would you do? Case 6 SBR 20 ,19 direct, 1 indirect Hb 15, wbc 8000 and platelets 300000 Mothers blood group O Rh positive, Baby’s O Rh positive Coombs test negative Ultrasound abdomen hepatomegaly, gallbladder not visualised HIDA scan Case 6 TFT raised TSH Urine for reducing substances Urine culture Other differentials Thank you