B. pertussis
advertisement

بسم هللا الرحمن الرحیم
Bordetella pertussis
http://www.hhmi.princeton.edu/sw/2002/psidelsk/Microlinks.htm
Roxana M.Ghanaie
Ped Infectious Disease
Subspecialist
Bordetella pertussis Basics
•
•
•
•
Aerobic, Gram negative coccobacillus
Alcaligenaceae Family
Specific to Humans
Colonizes the respiratory tract
– Whooping Cough (Pertussis)
Bordetella pertussis
is a bacterium identified in 1900 by
Jules Bordet and Octave Gengou but
isolated only in 1906 because of the
development of a medium containing
potatoes extract and rabbit blood
Jules Bordet
1870-1961
Estimated annual childhood deaths, 2002
Meningococcal (< 1%)
rotavirus (16%)
pneumococcal (28%)
76%
24%
measles (21%)
Hib (15%)
pertussis (11%)
tetanus (8%)
{
yellow fever (1%)
diphtheria (<1%)
polio (< 1%)
10.5 million deaths under 5 years of age
1.4 million from diseases where vaccination is currently available
1.1 million from diseases where vaccines will be available by 2008
Source: WHO/IVB
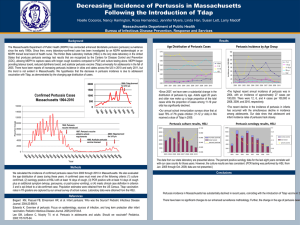
Reported Pertussis Cases
U.S., 1922-2003*
12,000
Number of cases
300,000
Number of cases
250,000
200,000
10,000
8,000
6,000
4,000
2,000
0
1980
150,000
1990
2000
100,000
50,000
0
1922 1930
1940
1950
1960
Year
1970
1980
1990
2000
Pertussis in a vaccinated country vs a non vaccinated country
Number of cases
Low vaccine coverage
*High morbidity and mortality in infants
*Regular asymptomatic contacts throughout life
*Unknown epidemiology in adults
1-2 3-4 5-6 7-12
2
3
Month
High vaccine coverage
*Low morbidity and mortality in infants
*Few asymptomatic contacts throughout life
*Increase in susceptible adolescents and adults
4
5
6
7 8-12 15-20 20-25 25-35
Year
Why speaking about Pertussis?
• Iran pertussis incidence 2010 : 0.5/ 100000
• DTP3 coverage more than 95%
روند میزان بروز سیاه سرفه محتمل و پوشش واكسن
ثالث نوبت سوم
(جمهوري اسالمي ايران )1370-1391
COVERAGE
95
1.4
90
1.2
85
1
80
0.8
75
0.6
70
0.4
65
0.2
60
0
13
70
13
71
13
72
13
73
13
74
13
75
13
76
13
77
13
78
13
79
13
80
13
81
13
82
13
83
13
84
13
85
13
86
13
87
13
88
13
89
13
90
13
91
DTP3
PERTUSSIS
INCEDENCE RATES/100.000
100
1.6
فراواني موارد محتمل سیاه سرفه برحسب
دانشگاه علوم پزشکی 1391
250
200
150
100
50
0
توزيع جغرافیايی موارد مثبت بیماری سیاه سرفه
دركشور 1391
20
15
10
5
0
Bordetella pertussis virulence determinants
TCT
TCT
BrkA,
Tcf,
Vag8
TCT
Pertussis toxin (PT)
Fimbriae
(FIM)
Pertactin
(PRN)
Filamentous
hemagglutinin
(FHA)
Adhesins: adhesion => multiplication
and colonisation of respiratory tract
Adenylate cyclase
hemolysin (AC-Hly)
Toxins: local and systemic
cytopathogenic effects
Classic Manifestation
• The incubation period of pertussis is usually 7 to
10 days, with a range of 4 to 21 days.
• The clinical course of illness is divided into three
stages.( age, vaccination, waning)
1/ The catarrhal stage is characterized by the onset
of runny nose, sneezing, low-grade fever, and a
mild cough. Cough gradually becomes more
severe (1-2 weeks)
Classic Manifestation
• 2/ The paroxysmal stage is characterized by
coughing fits (paroxysms), which may be
followed by a high-pitched inspiratory whoop,
vomiting, and/or apnea. (1-6 weeks), but may
continue for 10 weeks
• 3/The convalescent stage is characterized by
fewer paroxysmal coughing episodes and
usually disappears in 2-3 weeks, but may
continue for months
Complications
• Losing weight, pneumonia, otitis, seizure,
encephalopathy, apnea
• Epistaxia, melena, subdural hematoma,
inguinal hernia, rectal prolapse,
Infants
The severity of pertussis and the rapidity of its
progression in young infants is effected by a
number of factors such as:
the presence of transplacentally acquired
maternal antibodies to B. pertussis,
the infectious dose of bacteria that the infant
receives,
co-infection with respiratory
viruses and perhaps genetic
factors related to the
pathogen or the infant.
Infants
Short catarrhal period, longer convalescence period
Cough,feeding abn, res distress,apnea,cyanosis,
bradycardia, whoop uncommon,
paroxysms and this may lead to apnea, gasp,
hypoxia and occasionally seizures
Initially the chest is clear on auscultation but in fatal
cases B. pertussis pneumonia is always present.
Co-infection with respiratory viruses (particularly
RSV and adenoviruses) can confuse the diagnoses
because of a bronchiolitic picture (air trapping and
expiratory distress).
Pertussis Among Adolescents and
Adults
• Accounts for up to 7-30% of cough illnesses
per year
• Disease often milder than in infants and
children
• Infection may be asymptomatic, or may
present as classic pertussis
• Cough may last 21 d, st. paroxysmal
Clinical manifestation in immunized
• Mild , unrecognized cough
• Prolonged cough
• Persons with mild disease may transmit the
infection
• Older persons often source of infection for
children
• Adults: sleep disturbances
syncope, incontinence, rib Fx,
pneumonia
Transmission
• Very Contagious, 80% secondary attack rate among
susceptible persons( even immunized)
• Transmission occurs via respiratory droplets, direct
contact with respiratory secretions from infected
individuals
• Parents are a common source of B. pertussis
infections for infants,
• grandparents, uncles ,
Aunts also provide another
potential source of infection
Transmission
Pertussis Infectious Period:
• Most infectious during the catarrhal (early) stage.
• Infectious during the first 21 days of cough if not treated
with appropriate antibiotic.
• No longer infectious after 5 days of treatment with
appropriate antibiotic
• Length of communicability: age, immunization status,
appropirate antibiotic therapy
• Isolation: standard, droplet
B. parapertussis
• B. parapertussis infection in humans can cause
unrecognized infection, mild pertussis, or
classic pertussis
• B. bronchisepica
DD prolonged cough
•
•
•
•
•
•
•
Adenovirus
Para influenza
Influenza A,B
M.pneumonia
RSV
C.trachomatis
C. pneumonia
DD prolonged cough
• spasmodic attacks of coughing may be
observed in children with:
• bronchiolitis, bacterial pneumonia, cystic
fibrosis, or tuberculosis. Afebrile Pneumonia
Syndrome
• The cough associated with: sinusitis, airway
foreign body
• Laboratory confirmation of pertussis is
difficult and delayed. Therefore, clinicians
need to make the diagnosis of pertussis
presumptively in patients with a history of
intense paroxysmal or chronic coughing with
or without whooping, color changes,
posttussive vomiting, incomplete or absent
pertussis vaccination, and finding of
lymphocytosis on laboratory examination.
CXR Indications
•
•
•
•
•
1/ <1y
2/ toxic
3/ progressive cough>3 w
4/ res distress
5/ probable underlying dis( CF, CHD,forign
body, Hilar LAD)
Chest Xray
•
•
•
•
•
•
Most common : Normal
Shaggy heart( central airway not periph)
Hyperinflation, hyper lucent lung
Micro athelectasia
Secondary bac. Pneumonia
Bronchiolitis oblitrans( adeno, influ, measles,
pertussis)
• pneumothorax
Diagnosis
• Isolation by culture , preferred method of
diagnosis(100% specificity)
• Although PCR more sensetive,culture may be
necessary for further case analysis including
evaluation for
antibiotic resistance and
molecular typing
http://medinfo.ufl.edu/year2/mmid/bms5300/images/d7053.jpg
•
•
•
•
•
Neg culture:
Previously immunized
Antibiotic usage
More than 3 w after cough onset
Bad-handled specimen
Definition:
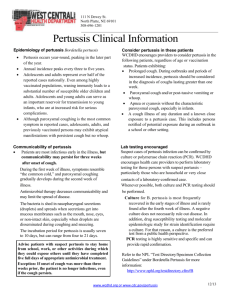
Clinical Case Definition of Pertussis
• A cough illness lasting at least 14 days with
one of the following:
• paroxysms of coughing,
• inspiratory “whoop”,
• or post-tussive vomiting,
• and without other apparent cause (as
reported by a health professional).
Definition:
Laboratory Criteria for Pertussis Diagnosis
• Isolation of Bordetella pertussis from a clinical
specimen (culture positive), or
• Positive polymerase chain reaction (PCR) assay for B.
pertussis DNA.
Note: Serological testing for B. pertussis is not
standardized
• Serology and DFA results should not be relied on as a
criterion for laboratory confirmation of pertussis.
Pertussis Case Classification
• Confirmed:
a/ A positive culture for B. pertussis and cough illness of any
duration, or
b/ Meets the clinical case definition and is confirmed by
PCR, or
c/ Meets the clinical definition and is epidemiologically
linked directly to a case confirmed by either culture or
PCR.
• Probable: A case that meets the clinical case definition, is not
laboratory confirmed, and is not epidemiologically linked to a
laboratory-confirmed case; also includes cases meeting the
outbreak case definition
Outbreaks
• Outbreak: Two or more cases involving two or more
households clustered in time (e.g., occurring within 42 days of
each other) and either epi-linked or sharing a common space
(e.g., in one building) where transmission is suspected to have
occurred (e.g. a school).
• One case in an outbreak must be lab confirmed (PCR positive
and meets case definition, or culture positive). In an outbreak
setting, a case may be defined as an acute cough illness
lasting ≥ 2 weeks without other symptoms.
Suspect: a clinical syndrome compatible with pertussis;
an illness consistent with pertussis and without other
apparent cause, such as:
• a. cough of ≥ 7 days, or
• b. paroxysmal cough of any duration, or
• c. cough with inspiratory whoop, or
• d. cough associated with apnea in an infant, or
• e. cough in a close contact of a confirmed or
probable case.
Summary of Pertussis Investigation and Control Guidelines Colorado Department of Public Health and Environment
Communicable Disease Epidemiology Program
مراقبت بیماري سیاه سرفه
ف ي
ت
ش .
ي
ي
ف
ي ي ش ل
ش.
ي
س
ح ل ال
ي آ
ط ح
ت.
ش
ي
ت ل
شگ
ش
ت
ي
ي
ش ع
شت
ل
ت
عش
،
ش
Management:
• The desired outcomes are:
1/ observing the severity of cough
2/ limiting the number of paroxysms,
3/ providing assistance when necessary,
4/ maximizing nutrition, rest, and recovery,
5/ follow the course of disease
6/ prevent/treat complications
• Admitt:
1- all infants<3 m despite severity & all 3-6 m except the
attacks are mild as observed by physician
2- with complications(intractable nausea and vomiting,
failure to thrive,seizures, encephalopathy, or for
patients with sustained hypoxemia during coughing
paroxysms who require supplemental oxygen,) hx of
prematurity in infant, with underlying cardiac, pul,
neuromuscular dis
Management
• For the hospitalized patient, in addition to
standard precautions, droplet precautions are
recommended
• Monitor heart rate, respiratory rate, and
oxygen saturation of hospitalized patients
continuously,especially in relation to coughing
paroxysms. Coughing, feeding, vomiting, and
weight changes should be recorded.
Management:
• Oxygen,suction,hydration, nutrition
• Patients who are severely ill may require treatment in an
ICU.
• Investigate all probable, pertussis reports.
• Recommend antibiotics for the index case (first case
reported to public health authorities), all household and
close contacts. Antibiotic inspite of age, immunization Hx
Report & find contacts
• Only confirmed and probable cases are reported.
• Recommend DTaP/Tdap vaccination according to
appropriate age for exposed children, adolescents
and adults.
• Exposed children < 7 years of age whose last DTP
( 4th dose) was more than 3 years ago should be
vaccinated.( more than 6m after 3rd dose)
Report & find contacts
• Evaluate close contacts for pertussis symptoms,
and when possible collect specimens for lab
testing from symptomatic persons
• Satisfactory documentation of disease:
recovery of B. pertussis on culture, OR typical symptoms and
clinical course when epidemiologically linked to a cultureproven case
Treatment (cont)
During catarrhal stage ameliorate disease
After cough establishment, does not generally
lessen duration; protect others
Limited benefit if begun >21 days after
onset/exposure
Exception: high risk cases/contacts treat up to 6 weeks
Treatment
• Antibiotic therapy
– Erythromycin
– Azithromycin
– Clarithromycin
http://www.aboutthatbug.com/AboutThatBug/files/CCLIBRARYFILES/
FILENAME/0000000032/033_lg.jpg
http://www.vet.purdue.edu/bms/courses/lcme510/chmrx/macrohd.htm
Treatment
Erythromycin
For children: 40-50 mg/kg/d in 4 divided
doses;10-14 days
• For adults: 1 to 2 g/day given every 6 h
Treatment
Azithromycin
• for children: at 10 mg/kg on day 1 and 5
mg/kg on days 2 to 5 as a single dose
for 5 days
• 10-12 mg/kg/d PO in 1 dose for a total of 5
days. ( < 6m)
• for adults: 500 mg on day 1 and 250 mg on
days2 to 5
Treatment
Clarithromycin
• for children: at 15 to 20 mg/kg/day in two
divided doses for 7 days
• for adults: 1 g/day in two doses for 7 days
Treatments
Trimethoprim(T)/Sulfamethoxazole (S)
8mg/kg T + 40 mg/kg S/d in 2
divided doses; 14 days
• Erythromycin and clarithromycin are not
recommended in infants younger than 4-6 w because
their use has been associated with increased risk for
infantile hypertrophic pyloric stenosis (IHPS).
• Resistant to macrolid: rare
• Cephalosporine, PN not effective
Treatment
• Humans infected with B. parapertussis or B.
holmesii
• macrolide therapy indicated above.
• In contrast, however, B. bronchiseptica is usually
resistant to Erythromycin Most sensitive to
aminoglycosides, extended-spectrum thirdgeneration penicillins, tetracyclines, quinolones,
and trimethoprim-sulfamethoxazole.
Treatment
• It has been observed in numerous small
studies that pertussis infant deaths relate
directly to the degree of leukocytosis
• double volume exchange transfusion, to lower
the white blood cell count
Treatment
• Pertussis-specific immune globulin is an
investigational product that may be effective
in decreasing paroxysms of
cough but requires further evaluation.
• The use of corticosteroids, albuterol, and
other beta2-adrenergic agents for the
treatment of pertussis is not
supported by controlled, prospective data
Exclusions from
work/school
Symptomatic: first 5 days of treatment
Symptomatic, refuses treatment: exclude for
21 days from onset of symptoms
Asymptomatic exposure: no exclusion
Complications in Infants
•
•
•
•
•
Pneumonia( in 22% infants)
Seizures( in 2% infants)
Encephalopathy( less than 0.5% infants)
FTT,Death 0.3%( 1% in less than 2 m-old)
SIDS( ???)
Prognosis
• Prognosis for full recovery is excellent; however, patients with
comorbid conditions as previously described have a
higher risk of morbidity and mortality
• Leukocytosis, particularly WBC counts of more than 100,000,
has been associated with fatalities from pertussis.
• Another study showed that WBC counts of more than
55, 000 and pertussis complicated by pneumonia were
independent predictors of fatal outcome in a multivariate
model.
Use a narrow definition of
close contact
Close contacts:
• Household contacts;
• Other persons having direct prolonged exposure to the
case while case was contagious and was coughing or
sneezing.
1. Direct face-to-face contact for an undefined time period
with an infectious pertussis case (case coughing < 21 days
and has not completed 5 days of appropriate antibiotic
treatment).
2. . Shared confined space in close proximity for a
prolonged period of time, such as ≥ 1 hour, with an
infectious pertussis case. For example, riding in a car with a
pertussis case.
3. Direct contact with respiratory, oral, or nasal secretions
from an infectious pertussis case (e.g., an explosive cough
or sneeze in the face, sharing food, sharing eating utensils,
kissing, mouth-to-mouth resuscitation, or performing a full
medical exam including examination of the nose and throat
without wearing a mask).
Summary of Pertussis Investigation and Control Guidelines Colorado Department of Public Health and Environment
Communicable Disease Epidemiology Program
Exposed
•
•
•
•
Household, close contacts, health care worker:
Check immunization, initiate, complete
Chemopx for all contacts regardless age, immunization
If start later than 21 d after exposure, give only to
highrisk: young infant, pregnant, care taker of infants
• Monitor for 21 d after last contact, for symptoms
• Evalute symptomatic exposed persons and exclude from
public setting and report confirmed, probable cases
QUESTIONS?
Diphtheria
[1
Etiology
• کورينه باکتريوم ديفتری باسیل گرم مثبت ،باريک ،چماقی
شکل ،بدون حرکت و بدون اسپور است که در رنگ آمیزی
بطور نامنظم رنگ میگیرد
• سويه های سم زای کورينه باکتريوم ديفتری ( باسیل
کلبس -لوفلر) و بندرت کورينه باکتريوم اولسرنس.
Etiology
•
•
•
•
•
4بیوتیپ ( میتیس ،اينترمديوس ،بلفانتی ،گراويس).
تمامی اين بیوتیپ ها می توانند توکسیکوژن باشند.
سم بیشتر توسط باسیل های جوانتر و در حال رشد و نمو
سريع تولید می شود.
سم ديفتری حتی در مقادير ناچیز 130میکروگرم بازای
کیلوگرم وزن بدن کشنده است
%99/9-94از انواع گراويس و انتر مديوس و حدود -80
%88انواع می تیس بیماريزا هستند.
Etiology
• خ
ف
• ک
یک
ع ت
ی7-2 :
ک
ت خ
ت.
لع ل یک .
Clinical Manifestation
• عالئم بسته به محل عفونت ،سطح ايمنی میزبان و انتشار
سیستمیک سم ان دارد.
• ديفتری بر اساس محل اناتومیک ورود عفونت و ايجاد
غشا به انواع :ديفتری مجاری بینی ،لوزه ها /حلق
( فارنکس) ،حنجره /الرنگو تراکه ،پوست و غیره تقسیم می
شود.
Clinical Manifestation
ف ژ ت غش ی
ت
ی ع ال
ی
•
ع ت
.
ی
ی
ال گ کئ ت
ی
بخ ف
ش ش ش
یش ، .
ظ ت ع ض 2-1
.
ع ال
پشت
غ،
ح ی ش ش.
ضعف
ی
خ ف ت
ضعی
ش ت ع ئ ع ی غ ب گی ش ت ض ع
.
Clinical Manifestation
• ديفتری قدامی بینی :در ابتدا بصورت سرماخوردگی با
ترشح رقیق از يک و يا هر دو بینی است و بدون عالئم
شديد سیستمیک است .ترشحات سپس غلیظ ،چرکی و بد
بومی شود .غشا سفید در داخل بینی ديده می شود .در
موارد شديد زخم ترشحی در پره های بینی و قسمت فوقانی
لب ديده میشود .حال عمومی معموال خوب است زيرا مقدار
کمی سم از مخاط بینی جذب می شود .بعلت وجود باسیل در
ترشح بینی ،خطر انتشار بیماری و ابتال به ديگران زياد
است .اين فرم بیشتر در شیرخواران وجود دارد.
Clinical Manifestation
• ديفتری لوزه و حلق :شروع بیماری تدريجی و با عالئم
غیر اختصاصی بی اشتهايی ،کوفتگی ،تب پايین و فارنژيت
است .غشا يک تا دو روز بعد ،از يک نقطه شروع شده و
کم کم غشا بخش اعظم هر دو لوزه را می گیرد.
• شدت گسترش ان بسته به وضعیت ايمنی
بیمار متغیر است.
• غشا رنگ زرد متمايل به خاکستری بوده
و بسختی به لوزه چسبندگی دارد.
• اغلب زبان کوچک درگیر است.
Clinical Manifestation
• در اثر نکروز غشا بوی دهان بسیار بد و نا مطبوع است.
غدد لنفاوی اکثرا بزرگ و حساس است.
• در اشکال شديد تورم غدد لنفاوی و نسوج نرم بصورت
تورم شديد گردن همراه با انسداد راههای هوايی فوقانی
بروز می کند .اين تورم گرم ،گوده گذار ،دردناک و سفت
است.
• بیشتر در کودکان باالی 6سال ديده می شود و معموال
توسط سويه های گراويس و اينترمديوس ايجاد می شود
Clinical Manifestation
• شدت عالئم بسته به میزان ازاد شدن توکسین و گسترش
غشا دارد.
• در موارد شديد ،کوالپس عروق ،کوالپس تنفسی،
خونريزی از بینی ،دهان ،گاه خونريزی منتشر و پورپورا
وجود دارد ،حال عمومی بد است و ظاهر بیمار رنگ پريده
و رنجور است تب وجود ندارد و يا خفیف است ولی تعداد
نبض بطور نامتناسب باال است.
•
•
•
•
ممکن است فلج کام بطور يکطرفه و يا دو طرفه ،اشکال
بلع و برگشت غذا از بینی وجود داشته باشد.
اختالل هشیاری،کوما ومرگ در عرض 7تا 10روز
اتفاق می افتد.
میوکارديت و نوروپاتی محیطی دارد .در موارد با شدت
کمتر ،بهبود آهسته تر است وگاه منجر به میوکارديت و
نوريت می شود .در موارد خفیف زمان بهبود متغیر است و
غشا در عرض 10-7روز کنده می شود.
عوارض ناشی از جذب توکسین در ديفتری حلق و لوزه
شديد تر از ديفتری ساير قسمتها است
دیفتری حنجره:
.
ف ی
ژ س طب ،
•
ی
یحق ت
• غبث
یش
ی س
ل
ش .غب
ی ،غش خ ی
خ فف ژت
ی
عث
ش
ت ی
ک پ ت.
ش .ع ئ ش
ع ضآ
ک
ذب ک
•
یش .
ل
ی
ت
Transmission
• بطور معمول انتشار از طريق قطرات و تماس با ترشحات
حلق ،بینی و پوست از بیمار و يا فرد ناقل انجام می شود.
• در صورت عدم درمان باسیل می تواند در تر شحات بینی
و يا حلق و يا در زخم پوست و يا چشم از 2تا 6هفته بعد
از آلودگی زنده بماند.
• در صورت درمان مناسب سرايت برای مدت کمتر از 4
روز امکان پذير است
Transmission
• انتقال ناشی ازتماس نزديک با بیماران و يا ناقلین
بخصوص در سفر به مناطق اندمیک و يا مسافرين از
مناطق اندمیک است.
• بندرت ديفتری از طريق اشیائ آلوده ،شیرخام ويا ساير
لبنیات منتقل می شود .در اثر جوشیدن شیر باسیل از بین
می رود
تعريف مورد بیماری
ی :هر بیم ری که ب ف ر ژیت،
ی
• ع ف
ال ر ژیت و ی تو سیلیت بهمر غش ئ چسب روی لوز
ه ،حلق و ی بی ی مر جعه م ی .
معیار اثبات ازمايشگاهی بیماری:
ک
ک
•
ف شح لچ
ی(
ی
ک ئ
ک
ی
ی
آ ی
ک
ک
ی
ل
ش)
گروه بندی موارد
ح ل :مور ی ست که معی ر ب لی ی ر شته ب ش .
•
طعی :مور ی که عالو بر معی ره ی ب لی ی ر ی
•
معی ره ی زم یش هی یز ب ش و ی رتب ط پی میولوژیک
ت یی ش ب مور ث بت ش ب لی ی شته ب ش .
ی کشت
ی
ی ک ف ع
:
•
ع
)
ثت ت(
.
ش
طعی
ح ل
Management
1/ Critical care needs
2/ Neutrilize toxin
3/ Eradicate C. diphtheria
4/ Complications
• Mechanical ventilation (combination of
airway obstruction by the diphtheritic
membrane and peripharyngeal edema )
Anti toxin
• Specific antitoxin is the mainstay of therapy
and should be administered on the basis of
clinical diagnosis
• neutralizes free toxin only.
• Efficacy diminishes with elapsing time after
the onset of mucocutaneous symptoms.
• Only an equine preparation is available
Anti toxin
• Antitoxin is administered once at an empiric
dose based on the degree of toxicity, site and
size of the membrane, and duration of illness.
• Most authorities prefer the intravenous route,
with infusion over 30-60 minutes.
Anti toxin
• Antitoxin is probably of no value for local
manifestations of cutaneous diphtheria, but
its use is prudent because toxic sequelae can
occur.
• Commercially available IVIG ,contain
antibodies to diphtheria toxin; is not proved
or approved
• Antitoxin is not recommended
for asymptomatic carriers.
Antitoxin
•
•
•
•
•
•
س حل
ی ع
ش ع
ش
ی ش
غش ی
یش :
ذب
ی ،ش ت
قی ض
ت
ث ت
ط
پ ی
ت
ش
ی 48
تک
ح
یحق
عت 40000-20000،ح
ف ژ ل 60000-40000ح
ی
ش
ت3
ی ش
120000-80000ح
ش
ی عضی 40000-20000
ی پ ی ع ال ث
یک
ح
Antimicrobial
• Eradication, prevent transmission, halt toxin production
• C diphtheriae is usually susceptible to various agents in vitro,
including penicillin,erythromycin, clindamycin, rifampin, and
tetracycline.
• Penicillin and erythromycin are only recommended for
treatment.
• Erythromycin is marginally superior to penicillin for
eradication of nasopharyngeal infection.
• Resistance to erythromycin is common in closed populations if
the drug has been used broadly
Antimicrobial
• ریترو م یسین خور کی و ی تزریقی بم ت 14روز( -40
50ب ز ی هر کیلوگرم وزن ،ح ثر 2گرم ر روز)
• پ ی سیلین Gتزریقی 100-150000 -و ح ب ز ی هر
کیلوگرم وزن م قطع ر 4وز) خل وری ی بر ی م ت
14روز
• پ ی سیلین Gپروک یین تزریقی عضال ی ( 25-50000
و ح ب ز ی هر کیلوگرم وزن ب ن روز ه ر و وز
م قسم) بم ت 14روز
Antimicrobial
• Antibiotic therapy is not a substitute for
antitoxin therapy.
• Elimination of the organism should be
documented by at least 2 successive cultures
from the nose and throat (or skin) obtained
24 h apart after completion of therapy.
• Treatment with erythromycin is repeated if
culture results remain positive
Vaccine
• Diseases dose not produce immunity,
vaccinate the patient in convalescent period
Surgical Care
• Otolaryngeal assessment is needed in patients
with severe respiratory or neurologic
complications or as part of critical care.
Consultation
Cardiologist:
Elevation of serum SGOT closely parallels the severity of
myonecrosis.
arise during the first 10 days of illness or may be delayed
until 2-3 weeks after
In electrocardiographic tracings, a prolonged PR
interval, changes in the ST-T wave, and single or
progressive cardiac dysrhythmias can occur, such as
first-degree, second-degree, and third-degree heart
block, atrioventricular dissociation, and ventricular
tachycardia. Toxic cardiomyopathy and myocarditis
• Neurologist:
• parallel the extent of primary infection and are
multiphasic in onset.
• Hypersthesia and local paralysis of the soft
palate
• Weakness of the posterior pharyngeal,
laryngeal, and facial nerves , causing a nasal
tone in the voice, difficulty in swallowing, and
risk of death from aspiration.
Neuropathy
• Cranial neuropathies characteristically occur in the
fifth week and lead to oculomotor and ciliary
paralysis, which manifest as strabismus, blurred
vision, or difficulty with accommodation.
• Symmetric polyneuropathy begins within 10 days to
3 months after oropharyngeal infection, motor
function deficit with diminished deep tendon
reflexes. DD polyneuropathy of Landry-Guillain-Barré
syndrome.
• Paralysis of the diaphragm can ensue.
Close contact
• Promptly identify close contacts of patients in
whom diphtheria is suspected. in the
household and other persons with a history of
habitual close contact with the patient.
Close contact
• For close contacts, irrespective of their immunization
status, the following measures should be taken:
• Surveillance for 7 days for evidence of disease
• Culture for C diphtheriae
• Antimicrobial prophylaxis with oral erythromycin (4050 mg/kg/d for 10 d; not to exceed 2 g/d) or a single
intramuscular injection of penicillin G benzathine
(600,000 U for children who weigh < 30 kg and 1.2
million U for children weighing >30 kg and adults)
Contacts
• Obtain repeated pharyngeal cultures from contacts proven to
be carriers at a minimum of 2 weeks after completion of
therapy.
• Asymptomatic, previously immunized, close contacts should
receive a booster dose of a preparation containing diphtheria
toxoid (DTaP, DT, Tdap, or Td, depending on age) if they have
not received a booster dose of diphtheria toxoid within 5
years. Immunize children in need of the fourth dose.
Contacts who cannot be kept under surveillance should receive
benzathine penicillin G (not erythromycin),
• and a dose of , DT, or Td (administered if the patient has not
received a booster injection within 1 year)
Mortality/Morbidity
• Death due to mechanical airway obstruction
or cardiac involvement with circulatory
collapse
• In at least 10% of patients with respiratory
tract diphtheria
Mortality/Morbidity
Prognosis depends on:
• The virulence of the organism (with the gravis
strain usually accounting for the most severe
disease),
• The age and immunization status of the patient,
• The site of involvement,
• The speed with which antitoxin is administered
Mortality/Morbidity
• Airway obstruction by the diphtheritic
membrane and peripharyngeal edema
combine to pose a risk of death in patients
with diphtheria.
Mortality/Morbidity
• For patients in whom disease is recognized on
day 1 and therapy is promptly initiated, the
mortality rate is approximately 1%.
• If appropriate treatment is withheld until day
4, the mortality rate rises to 20%
Mortality/Morbidity
• Toxic cardiopathy occurs in approximately 1025% of patients with diphtheria and is
responsible for 50-60% of deaths.
• Neurologic complications parallel the extent
of primary infection and are multiphasic in
onset.
مراقبت بیماری ديفتری
یپئ
ت
ک
• کش
ت
پ شش ی ش 90
ی
ح ل طعی
ط عت
ش
ت
ال
ط حپئ
یش .ط عت
ف ی ی
ی
تپ ش
ت ی
یک ل
ث خشی
ع
ک .
اقدامات الزم در اولین برخورد با
بیمارمحتمل به ديفتري
ش
-
ي
ف ي
ي
ظ
ل
پس
آ
خ
قآ
قآ
ي
ش
شت
.
ك ي
شت
ب
شح ت ح ق
ش 14
ي
.
ح ب حل ض ع
پ ئ
كپ
.
ت 14
غ
ف
ي
ش ت
ي
ط
TREND OF PROBABLE DIPHTERIA CASES
INCEDENCE RATES
& DTP3 COVERAGE (I.R.IRAN 1370-1391)
0.9
98
0.8
96
0.7
94
0.6
92
0.5
90
0.4
88
0.3
0.2
86
0.1
84
0
82
DIPHTERIA
DTP3
COVERAGE
100
13
70
13
71
13
72
13
73
13
74
13
75
13
76
13
77
13
78
13
79
13
80
13
81
13
82
13
83
13
84
13
85
13
86
13
87
13
88
13
89
13
90
13
91
INCEDENCE RATE/100.000
1
فراواني موارد محتمل ديفتری برحسب
دانشگاه علوم پزشکی 1391
140
120
100
80
60
40
20
کشن
ک
س
ک من
ک م
گل ن
گ الن
ل س ن
س ری
ر
م ه
ه م گن
ه ن
روم ه
رب
هن
ه ز
یالم
بب
ب شه
ب ج
ت ی
زب
وی
ی
روم ه
رب
هن
ه ز
یالم
بب
ب شه
ب ج
ت ی
ته ن
جه م
ب ری
ب ر
ز ن
س ور
س ن
شه و
شه به ی
ش ز
وی
0
QUESTIONS?