Nov 2012 Pertussis - CA Presentation
advertisement

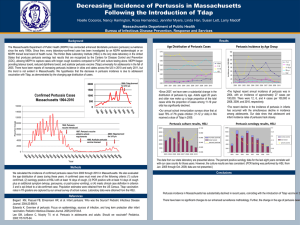
Pertussis Overview Claudia Alvarado RN BSN Public Health Nurse Coordinator Department of Public Health Services First recognized in the 16th Century Caused by bacteria Bordetella Pertussis Pertussis bacteria produces toxins which are responsible for clinical features of illness Pertussis epidemics cyclic every 2-5 years Effectively treated with Antibiotic Closely related organism: Bordetella para-pertussis • Incubation period: usually 7-10 days (range 6-21 days) • Infectious Period: Begins with onset of the catarrhal stage or onset of cough and ends 21 days after cough onset or 5 days of treatment with appropriate antibiotic. • Mode of transmission: Person-to person through aerosolized droplets or by direct contact with secretions from the respiratory tract Susceptibility: Highly contagious with a > 80% secondary attack rate among susceptible persons in a households Pertussis occurs at any age regardless of vaccine status Vaccine immunity to pertussis wanes in 5-10 years, may be less with acellular vaccine (data very limited) Catarrhal stage: Onset often insidious with cold like symptoms usually for 1-2 weeks with gradually increasing cough Paroxysmal stage: Paroxysms, inspiratory whoop, vomiting, apnea, cyanosis (often after paroxysms) usually for 1-6 weeks, up to 10 weeks Convalescent stage: Mild cough for weeks to months • Symptoms in vaccinated persons are milder • Less characteristic symptoms in adolescent and adults • Infants 6 months and younger have atypical presentation – Shorter catarrhal stage – Gagging, gasping, apnea, less often paroxysms – Whoop may be absent Infants <12 months: Hospitalization ( 50%) Apnea (50%) Bacterial Pneumonia (20%) Seizures (1%) Death (1%) Encephalopathy (1%) • CDC/CSTE Clinical Case Definition (Probable Case) – a cough illness lasting at least 2 weeks with one of the following: paroxysms of coughing, inspiratory "whoop," or post- tussive vomiting AND – without other apparent cause (as reported by a health-care professional) • CDC/CSTE Laboratory/Confirmatory Criteria for Diagnosis – isolation of Bordetella pertussis from a clinical specimen OR – positive polymerase chain reaction (PCR) assay for B. pertussis OR – Epidemiologic link to laboratory confirmed case <3 weeks = acute (URI, CHF, PE) 3-8 weeks = subacute (persistent URI, lung cancer) >8 weeks = chronic (asthma, reflux disease) Adenoviruses, Mycoplasma pneumoniae, RSV,Chlamydia pneumoniae Consider in Pertussis even if patient is immunized PCR, culture, serology (not accepted, except when done by MA PHL) CDC recommends Nasopharyngeal swabs be tested for PCR and Culture, as PCR prone to false positives Use Dacron tipped NP swab with flexible wire handle Do not use Cotton or Calcium-Alganate swabs Use Regan-Lowe transport media Mask and gloves Azithromycin for 5 days is effective Treatment (all age groups, recommended for infants <1 month) Erythromycin for14 days (not preferred in infants less than one month) Clarithromycin for for 7 days, not recommended for infants <1 month TMP/SMC for 14 days, contraindicated in infants < 6 months Direct contact with oral, nasal, or respiratory secretions from a symptomatic patient Direct face to face exposure with a symptomatic case Sharing the same confined space in close proximity with a symptomatic patient for an hour or more Performing bronchoscopy, suctioning, exam of mouth, nose or throat and mouth to mouth resuscitation (droplet) Contact groups: i.e. household, friends, school, car/bus religious groups, sports teams, social events, and…. Healthcare HIGH RISK CONTACTS: Use more inclusive criteria for definition of close contact Infants less than one year of age, especially less than six months of age Persons with underlying medical conditions such as chronic lung disease, respiratory insufficiency and cystic fibrosis Persons with immune deficiencies (including HIV) Protect infants by: Protecting from known/suspect cases Liberal use of term close contact and PEP for infants and persons around them Vaccinating “around” infant Pregnant women, especially in the third trimester due to the increased risk to a newborn infant, as well as other pregnant women (i.e. in medical setting) Health Care workers providing direct patient care, especially prenatal care, labor and delivery, neonatal and pediatric fields Babysitter/daycare worker taking care of infants Parents/Parents to be/Caregivers of infants For Patient: Exclusion/Isolation until completion of 5 days on ABX or 21 days post cough onset (whichever is sooner) For non-symptomatic contacts: Post Exposure Prophylaxis (PEP) For symptomatic contacts: Evaluation (including NP for PCR and/or CX) and PEP/TX/Exclusion as appropriate High risk contacts should be started on PEP up to 42 days of exposure Household: All should be on PEP or TX Home child care: Treat children as household contacts Childcare center: PEP depending on amount of contact/age Pregnant Contacts: Pregnant women and persons close to them should be started on PEP for up to 6 weeks after last exposure to pertussis. Especially important during the last trimester due to increased risk for a infant, if exposed. Droplet precautions (if mom and infant on ABX rooming together and breastfeeding encouraged) Clinical/Outpatient settings: Most individuals in waiting rooms etc. with a Pertussis case should not be considered close contacts. Persons who had direct contact with respiratory secretions from the case or intense close contact may be considered for PEP Facilities/Institutions: (i.e. Nursing Homes and institutions for developmentally disabled): Residents have multiple sources of exposure and increased risk of complications More inclusive interpretation of “close” contacts may be indicated. Hospital setting: Determination of close contact should be more inclusive in settings such as a neonatal intensive care unit, newborn nursery, or infant ward, because infants are at risk for developing severe disease Health Care Workers (HCWs) and Patients should be considered exposed only if the source is a confirmed case, or a suspect case during an outbreak. HCWs should wear a mask for respiratory protection. Patients and HCWs exposed to pertussis, should be questioned about symptoms of cough illness, and be instructed to report the development of symptoms within 42 days of exposure to infection control staff. If symptomatic, Health Care Worker (HCW) should be cultured for pertussis, treated and excluded for the first 5 days of a full course of appropriate antibiotic treatment. If a symptomatic HCW cannot take or refuses antimicrobial therapy, the HCW should be excluded for 21 days after the onset of cough. The use of a mask by the HCW does not provide adequate protection during this time. Active surveillance in health care settings should continue for 42 days after the onset of cough of the last case of pertussis. Year Reported Cases* 2000 7,867 2001 7,580 2002 9,771 2003 11,647 2004 25,827 2005 25,616 2006 15,632 2007 10,454 2008 13,278 2009 16,858 2010 27,550 2011* 18,719 *Total reported cases include those with unknown age http://www.cdc.gov/pertussis/survreporting.html Wisconsin 87.6 Utah 33.6 27 Arizona Idaho 12.2 Minnesota 72.6* New Mexico 12 Washington Vermont Montana 23.5 21.9 17.2 Pennsylvania Missouri Colorado 11.7 11.6 11 Maine Iowa 62.3 Alaska 51.9 Oregon 44.7 Kansas New 42.6 Hampshire 42.1 New York 14.9 13.8 Kentucky Wyoming 10.7 10.3 North Dakota 41.9 Illinois 12.3 Nebraska 8.8 Year 2007 2008 2009 2010 2011 2012 Cases 79 44 79 22 171 184 Incidence per 100.000 6 3 6 2 12 15 In Household: Two or more cases, with at least one case being confirmed. This definition may be used to count cases/surveillance purposes. Other settings (i.e. School, Daycare, Health Care):Two or more cases clustered in a setting and time (within 42days of each other), one of which has been confirmed. Community Outbreak: A higher than expected number of reported cases in a population in a defined time period on the basis of previously reported disease numbers during a non epidemic time period (historical disease patterns) Institution of droplet precautions in addition to standard precautions for suspect and known cases Cohort exposed patients PEP for exposed employees and patients Evaluate all symptomatic exposed employees, treat and exclude until on TX x 5 days or 21 days post cough onset Active surveillance x 42 days after onset of cough of last case of pertussis Education of high risk units via in-service Education of other staff via fact sheets, other communications Evaluation of staff with respiratory illness Cohort patients with cough illness Restriction of patients to affected floor, masking when leaving floor Consideration of requirement for visitors to wear surgical mask while in facility Consideration of vaccination for exposed staff Immunization of Health-Care Personnel Recommendations of the Advisory Committee on Immunization Practices (ACIP) http://www.cdc.gov/mmwr/pdf/rr/rr6007.pdf Recommended Adult Immunization Schedule— United States - 2012 http://www.cdc.gov/vacc ines/schedules/downloa ds/adult/adultschedule.pdf Report on Pertussis Epidemic –Washington 2012 2,520 confirmed and probable cases of pertussis (83.4% confirmed) between January 01 and June 16 2012 Review done with attention to Immunization status of patients Vaccinate HCP regardless of age with a single dose of Tdap as soon as feasible if no prior dose No minimal interval between last Td and Tdap for HCW Hospitals and ambulatory-care facilities should provide Tdap for HCWs and maximize immunization rates THANK YOU!