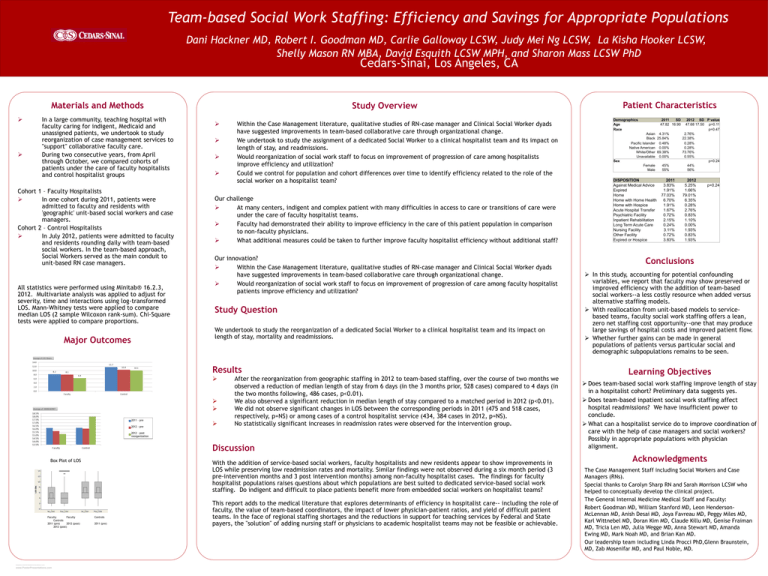
Team-based Social Work Staffing: Efficiency and Savings for Appropriate Populations
Dani Hackner MD, Robert I. Goodman MD, Carlie Galloway LCSW, Judy Mei Ng LCSW, La Kisha Hooker LCSW,
Shelly Mason RN MBA, David Esquith LCSW MPH, and Sharon Mass LCSW PhD
Cedars-Sinai, Los Angeles, CA
Materials and Methods
In a large community, teaching hospital with
faculty caring for indigent, Medicaid and
unassigned patients, we undertook to study
reorganization of case management services to
"support" collaborative faculty care.
During two consecutive years, from April
through October, we compared cohorts of
patients under the care of faculty hospitalists
and control hospitalist groups
Cohort 1 – Faculty Hospitalists
In one cohort during 2011, patients were
admitted to faculty and residents with
'geographic' unit-based social workers and case
managers.
Cohort 2 – Control Hospitalists
In July 2012, patients were admitted to faculty
and residents rounding daily with team-based
social workers. In the team-based approach,
Social Workers served as the main conduit to
unit-based RN case managers.
All statistics were performed using Minitab® 16.2.3,
2012. Multivariate analysis was applied to adjust for
severity, time and interactions using log-transformed
LOS. Mann-Whitney tests were applied to compare
median LOS (2 sample Wilcoxon rank-sum). Chi-Square
tests were applied to compare proportions.
Within the Case Management literature, qualitative studies of RN-case manager and Clinical Social Worker dyads
have suggested improvements in team-based collaborative care through organizational change.
We undertook to study the assignment of a dedicated Social Worker to a clinical hospitalist team and its impact on
length of stay, and readmissions.
Would reorganization of social work staff to focus on improvement of progression of care among hospitalists
improve efficiency and utilization?
Could we control for population and cohort differences over time to identify efficiency related to the role of the
social worker on a hospitalist team?
Our challenge
At many centers, indigent and complex patient with many difficulties in access to care or transitions of care were
under the care of faculty hospitalist teams.
Faculty had demonstrated their ability to improve efficiency in the care of this patient population in comparison
to non-faculty physicians.
What additional measures could be taken to further improve faculty hospitalist efficiency without additional staff?
Our innovation?
Within the Case Management literature, qualitative studies of RN-case manager and Clinical Social Worker dyads
have suggested improvements in team-based collaborative care through organizational change.
Would reorganization of social work staff to focus on improvement of progression of care among faculty hospitalist
patients improve efficiency and utilization?
Study Question
We undertook to study the reorganization of a dedicated Social Worker to a clinical hospitalist team and its impact on
length of stay, mortality and readmissions.
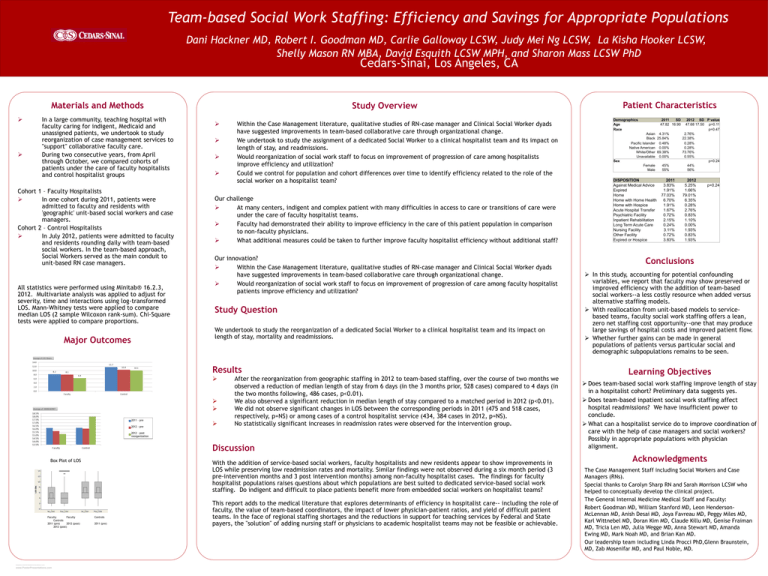
Major Outcomes
Results
2011 – pre
2012 - pre
After the reorganization from geographic staffing in 2012 to team-based staffing, over the course of two months we
observed a reduction of median length of stay from 6 days (in the 3 months prior, 528 cases) compared to 4 days (in
the two months following, 486 cases, p<0.01).
We also observed a significant reduction in median length of stay compared to a matched period in 2012 (p<0.01).
We did not observe significant changes in LOS between the corresponding periods in 2011 (475 and 518 cases,
respectively, p=NS) or among cases of a control hospitalist service (434, 384 cases in 2012, p=NS).
No statistically significant increases in readmission rates were observed for the intervention group.
2012 – post
reorganization
Discussion
Box Plot of LOS
Faculty
Faculty
Controls
2011 (pre)
2012 (post)
2012 (post)
RESEARCH POSTER PRESENTATION DESIGN © 2012
www.PosterPresentations.com
With the addition of service-based social workers, faculty hospitalists and new residents appear to show improvements in
LOS while preserving low readmission rates and mortality. Similar findings were not observed during a six month period (3
pre-intervention months and 3 post intervention months) among non-faculty hospitalist cases. The findings for faculty
hospitalist populations raises questions about which populations are best suited to dedicated service-based social work
staffing. Do indigent and difficult to place patients benefit more from embedded social workers on hospitalist teams?
Controls
2011 (pre)
Patient Characteristics
Study Overview
This report adds to the medical literature that explores determinants of efficiency in hospitalist care-- including the role of
faculty, the value of team-based coordinators, the impact of lower physician-patient ratios, and yield of difficult patient
teams. In the face of regional staffing shortages and the reductions in support for teaching services by Federal and State
payers, the "solution" of adding nursing staff or physicians to academic hospitalist teams may not be feasible or achievable.
Demographics
Age
Race
2011
SD
47.82 16.90
45%
55%
2012 SD P value
47.68 17.50 p=0.11
p=0.47
2.76%
22.38%
0.28%
0.28%
73.76%
0.55%
p=0.24
44%
56%
2011
3.83%
1.91%
77.03%
6.70%
1.91%
1.67%
0.72%
2.15%
0.24%
3.11%
0.72%
3.83%
2012
5.25%
1.66%
79.01%
6.35%
0.28%
2.76%
0.83%
1.10%
0.00%
1.93%
0.83%
1.93%
Asian 4.31%
Black 25.84%
Pacific Islander 0.48%
Native American 0.00%
White/Other 69.38%
Unavailable 0.00%
Sex
Female
Male
DISPOSITION
Against Medical Advice
Expired
Home
Home with Home Health
Home with Hospice
Acute Hospital Transfer
Psychiatric Facility
Inpatient Rehabilitation
Long Term Acute Care
Nursing Facility
Other Facility
Expired or Hospice
p=0.24
Conclusions
In this study, accounting for potential confounding
variables, we report that faculty may show preserved or
improved efficiency with the addition of team-based
social workers--a less costly resource when added versus
alternative staffing models.
With reallocation from unit-based models to servicebased teams, faculty social work staffing offers a lean,
zero net staffing cost opportunity--one that may produce
large savings of hospital costs and improved patient flow.
Whether further gains can be made in general
populations of patients versus particular social and
demographic subpopulations remains to be seen.
Learning Objectives
Does team-based social work staffing improve length of stay
in a hospitalist cohort? Preliminary data suggests yes.
Does team-based inpatient social work staffing affect
hospital readmissions? We have insufficient power to
conclude.
What can a hospitalist service do to improve coordination of
care with the help of case managers and social workers?
Possibly in appropriate populations with physician
alignment.
Acknowledgments
The Case Management Staff including Social Workers and Case
Managers (RNs).
Special thanks to Carolyn Sharp RN and Sarah Morrison LCSW who
helped to conceptually develop the clinical project.
The General Internal Medicine Medical Staff and Faculty:
Robert Goodman MD, William Stanford MD, Leon HendersonMcLennan MD, Anish Desai MD, Joya Favreau MD, Peggy Miles MD,
Karl Wittnebel MD, Doran Kim MD, Claude Killu MD, Genise Fraiman
MD, Tricia Len MD, Julia Wegge MD, Anna Stewart MD, Amanda
Ewing MD, Mark Noah MD, and Brian Kan MD.
Our leadership team including Linda Procci PhD,Glenn Braunstein,
MD, Zab Mosenifar MD, and Paul Noble, MD.