What Did We Learn? - UNM Hospitalist Wiki
advertisement
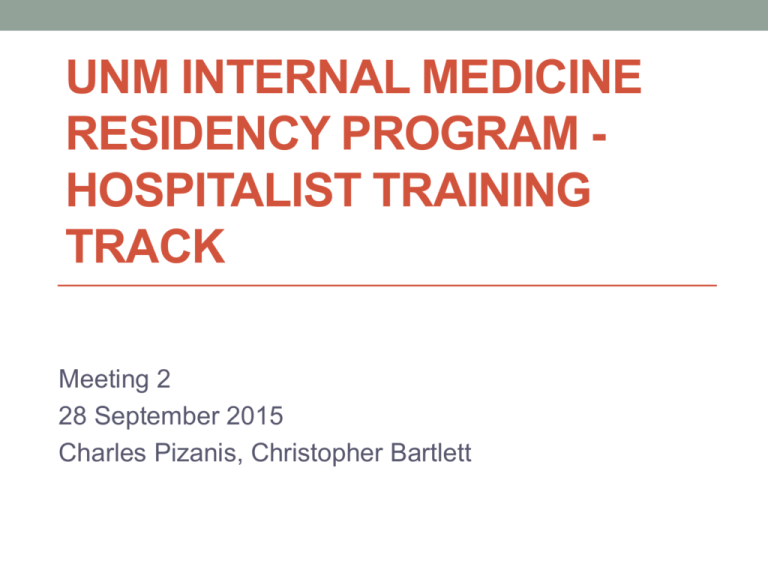
UNM INTERNAL MEDICINE RESIDENCY PROGRAM HOSPITALIST TRAINING TRACK Meeting 2 28 September 2015 Charles Pizanis, Christopher Bartlett Objectives • Describe hospitalist training track concept • Share results of needs assessment of former UNM IM grads • Review vision and structure of training track at UNM • Decide on required rotations, format of small group curriculum, any additional elements of track Hospitalist Training Tracks • Programs across country have developed training tracks to provide training, exposures residents interested in hospital medicine • Tracks share clinical rotations, small group meetings, quality/research experiences • Graduates of these tracks go on to become community hospitalists, academic hospitalists, and leaders in hospital medicine Needs Assessment Why Did We Do It? By understanding the strengths and weaknesses of the UNM Internal Medicine Residency Program, from the perspective of current hospitalist physicians, a Hospitalist Training Pathway curriculum can be developed to meet and exceed the needs of future graduates entering academic and community hospitalist medicine. Who Did We Contact? All UNM Internal Medicine graduates within the past 3 years who are currently employed as an academic and/or community hospitalist physician. Hospitalist Training Track - Needs Assessment Results ID Q1 Q2 Q3 Q4 Q5 1 4 Neuro, ID, Consult 4.0 3.0 3.0 2 5 Hosp Admin, Periop, Overseeing Res Teams 3.0 4.0 1.0 3 3 QI, Consult, Rehab Services (WC, PT), Financial Aspects of Medicine 5.0 4.0 2.0 4 4 Financial Aspects of Medicine, High Value Care, Private Practice Exposure 5.0 4.0 1.0 5 5 Hosp Admin, Conflict Resolution/Team Building, Neuro (CVA+Seizure), Med Education 5.0 5.0 4.0 6 4 Procedure Team, High Value Care, ID, QI 4.0 5.0 2.5 7 4 Medical Economics, Procedure Team, Neurology 5.0 3.0 2.5 8 4 Cardiology, Neurology, 2.0 1.0 1.0 9 4 Scholarly Activity, QI 4.0 4.0 1.0 What Did We Learn? Question 1: Internal Medicine residency at the University of New Mexico fully prepared me to become a hospitalist physician. 7 6 # of Responses 6 5 4 3 2 2 1 1 0 1 2 3 4 5 Perception – 1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree A majority of respondents agree or strongly agree that their residency experience fully prepared them for careers in hospital medicine. What Did We Learn? Question 2: In which aspects of your job as a hospitalist today do you wish you had received more training during residency? Neurology 22% 44% Infectious Disease Consultative/Perioperative Medicine 44% 22% Medical Education Medical Economics 22% 33% Hospital Administration Quality Improvement/High Value Care 33% 33% Procedure Team Respondents believe they would have benefited from more training in Neurology (44%), Quality Improvement/High Value Care (44%), Consultative/Perioperative Medicine (33%), Medical Education (33%), and Medical Economics (33%). What Did We Learn? Question 3: A Hospitalist Pathway could have filled these gaps? 5 4 # of Responses 4 3 3 2 1 1 2 3 1 0 1 4 5 Perception – 1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree A majority of respondents agree of strongly agree that a Hospitalist Pathway could have filled perceived gaps in their education. What Did We Learn? Question 4: I would have considered participating in a Hospitalist Pathway? 5 4 # of Responses 4 3 2 2 2 1 1 0 1 2 3 4 5 Perception – 1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree A majority of respondents agree of strongly agree that they would have considered participating in a Hospitalist Pathway. What Did We Learn? Question 5: How many electives per year would you have been willing to exchange in order to take part in a Hospitalist Pathway? 5 # of Responses 4 4 3 2 2 1 1 1 1 3 4 0 1 2 2-3 A majority of respondents felt like they would be willing to exchange 1 elective in order to take part in a Hospitalist Pathway. The average and median were 2. What Did We Learn? 1.A majority of respondents agree or strongly agree that their residency experience fully prepared them for careers in hospital medicine. 2.Respondents believe they would have benefited from more training in Neurology (44%), Quality Improvement/High Value Care (44%), Consultative/Perioperative Medicine (33%), Medical Education (33%), and Medical Economics (33%). 3.A majority of respondents agree of strongly agree that a Hospitalist Pathway could have filled perceived gaps in their education. 4.A majority of respondents agree of strongly agree that they would have considered participating in a Hospitalist Pathway. 5.A majority of respondents felt like they would be willing to exchange 1 elective in order to take part in a Hospitalist Pathway. The average and median were 2. UNM Internal Medicine Residency Hospitalist Training Track Overview Clinical Rotations • • • • Consultative Medicine (UNMH) SRMC Hospitalist (SRMC) Medical Economics (UNMH) Palliative Care Consults QI/Research Project • Project chosen by resident • Guidance by QI/research mentor • Goal of presentation at conference and/or publication of project Mentorship • Paired hospitalist mentor • Career mentoring • Leadership mentoring • HTT director mentor Didactic Curriculum • Small group meetings • Online Society of Hospital Medicine (SHM) modules • Online Institute for Healthcare Improvement (IHI) Open School curriculum Track Basics • 2-4 track participants per year • Application process to begin in PGY1 year • Track to occur over PGY2 - PGY3 HTT Track Timeline PGY 1 • Apply to HTT (January) • Acceptance to track (mid February) • Select PGY2 schedule (Spring) • Meet with HTT director (Spring) • Meet with QI/research mentor and decide on project (late Spring) PGY 2 PGY 3 • Begin required HTT rotations • Begin work on project • Begin SHM/IHI curriculum • Attend scheduled small group curriculum lectures • Meet with QI/research mentor (quarterly) • Attend one regional, one national conference • Select PGY3 schedule (Spring) • Complete required HTT rotations • Meet with research/QI mentor (quarterly) • Complete work on project (Fall, Spring) • Submit scholarly work (Fall, Spring) • Complete SHM/IHI curriculum • Attend one regional, one national conference • Complete HTT Clinical Rotations – How Many and Which Ones? • Consultative Medicine (UNMH) • Grow in skills as medical consultant, increase exposure to perioperative care • SRMC Hospitalist (SRMC) • Provide exposure to work as community hospitalist • Medical Economics (UNMH) • Increase knowledge and understanding of business and economics principles of medicine • Palliative Care Consults • Provide additional exposure to palliative and end-of-life care Small Group Curriculum • Format • Topics brainstorm • Journal Club • Schedule • Monthly vs every-other month Any Additional Elements We Should Include? Timeline of Rollout 2015 • November meeting • September meeting • Review track curriculum • Decide on rotations, • December meeting format of small group • Finalize track curriculum curriculum, additional • Dec 31 elements • Completed curriculum, • Start work on curriculum structure, materials for • October – retreat rotation • Report back on progress of additional elements 2016 • Solicit speakers for topics • January - applications • Solicit QI/research mentors Thanks!