ppt - Click here to
advertisement
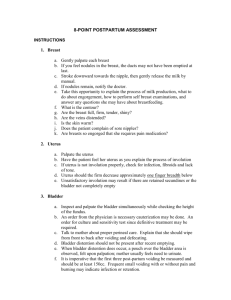
Postpartum Nursing Care BY: DR MEHARUNNISSA KHASKHELI Pathophysiology of Postpartum Involution - rapid reduction in size of uterus and return to pre-pregnant state Subinvolution = failure to descent Uterus is at level of umbilicus within 6 to 12 hours after childbirth - decreases by one finger breadth per day Exfoliation - allows for healing of placenta site and is important part of involution – may take up to 6 weeks Enhanced by uncomplicated labor and birth complete expulsion of placenta or membranes breastfeeding early ambulation FIGURE 23–1 Involution of the uterus. A, Immediately after expulsion of the placenta, the top of the fundus is in the midline and approximately halfway between the symphysis pubis and the umbilicus. B, About 6 to 12 hours after birth, the fundus is at the level of the umbilicus. The height of the fundus then decreases about one finger breadth (approximately 1cm) each day. Pathophysiology of Postpartum Uterus rids itself of debris remaining after birth through discharge called lochia Lochia changes: Bright red at birth Rubra - dark red (2 – 3 days after delivery) Serosa – pink (day 3 to 10 after delivery) Alba – white Clear If blood collects and forms clots within uterus, fundus rises and becomes boggy (uterine atony) Ovulation and Menstruation/Lactation Return of ovulation and menstruation varies for each postpartal woman Menstruation returns between 6 and 10 weeks after birth in nonlactating mother - Ovulation returns within 6 months Return of ovulation and menstruation in breastfeeding mother is prolonged related to length of time breastfeeding continues Breasts begin milk production a result of interplay of maternal hormones Pathophysiology of Bowel Elimination Intestines sluggish because of lingering effects of progesterone and decreased muscle tone Spontaneous bowel movement may not occur for 2 to 4 days after childbirth Mother may anticipate discomfort because of perineal tenderness or fear of episiotomy tearing Elimination returns to normal within one week After cesarean section, bowel tone return in few days and flatulence causes abdominal discomfort Pathophysiology of Urinary tract Increased bladder capacity, decreased bladder tone, swelling and bruising of tissue Puerperal diuresis leads to rapid filling of bladder urinary stasis increases chance of urinary tract infection If fundus is higher than expected on palpation and is not in midline, one should suspect bladder distension Laboratory Values White blood cell count often elevated after delivery Leukocytosis Elevated WBC to 30,000/mm3 Physiologic Anemia Blood loss – 200 – 500 Vaginal delivery Blood loss 700 – 1000 ml C/S RBC should return to normal w/in 2 - 6 weeks Hgb – 12 – 16, Hct – 37% - 47% Activation of clotting factors (PT, PTT, INR) predispose to thrombus formation - hemostatic system reaches non-pregnant state in 3 to 4 weeks Risk of thromboembolism lasts 6 weeks Weight Loss 10 –12 pounds with delivery 5 pounds with diuresis Return to normal weight by 6 – 8 weeks if gained 25 - 30 pounds Breastfeeding will assist with weight loss even with extra calorie intake Psychosocial Changes Taking in - 1 to 2 days after delivery Mother is passive and somewhat dependent as she sorts reality from fantasy in birth experience Food and sleep are major needs Taking hold - 2 to 3 days after delivery Mother ready to resume control over her life She is focused on baby and may need reassurance Psychosocial Changes Maternal Role Attachment Woman learns mothering behaviors and becomes comfortable in her new role Four stages to maternal role attainment Anticipatory stage - During pregnancy Formal stage - When baby is born Informal stage - 3 to 10 months after delivery Personal stage - 3 to 10 months after delivery Father-Infant Interaction Engrossment Sense of absorption Preoccupation - Interest in infant Postpartum Assessment Vital signs: Temperature elevations should last for only 24 hours – should not be greater than 100.4°F Bradycardia rates of 50 to 70 beats per minute occur during first 6 to 10 days due to decreased blood volume Assess for BP within normal limits: Notify for tachycardia, hypotension, hypertension Respirations stable Breath sounds should be clear Complete systems assessment Postpartum chills or shivers are common Breasts Assessment Assess if mother is breast- or bottle-feeding - inspect nipples and palpate for engorgement or tenderness – should not observe redness, blisters, cracking Breasts Assessment Breasts should be soft, warm, non-tender upon palpation Secrete colostrum for 1st 2-3 days –yellowish fluid protein and antibody enriched to offer passive immunity and nutrition Milk comes in around 3 – 4 days – feel firm, full, tingly to client Uterus Assessment Monitor uterus and vaginal bleeding, every 30 minutes for first PP hour, then hourly for 2 more hours, every 4 hours, then every 8 hours or more frequently if there is bogginess, position out of midline, heavy lochia flow Determine firmness of fundus and ascertain position approximate descent of 1 cm or 1 fingerbreadth per day If boggy (soft), gently massage top of uterus until firm – notify health care provider if does not firm Displaced to the right or left indicates full bladder – have client void and recheck fundus Uterus Assessment FIGURE 23–6 Measurement of descent of fundus for the woman with vaginal birth. The fundus is located two finger-breadths below the umbilicus. Always support the bottom of the uterus during any assessment of the fundus. Bladder and Bowel Assessment Anesthesia or edema may interfere with ability to void – palpate for bladder distention - may need to catheterize – measure voided urine Assess frequency, burning, or urgency Diuresis will occur 12 – 24 hours after delivery – eliminate 2000 – 3000 ml fluid, may experience night sweats and nocturia Bowel: Assess bowel sounds, flatus, and distention Lochia – Rubra Assessment Lochia = blood mucus, tissue vaginal discharge Assess amount, color, odor, clots If soaking 1 or > pads /hour, assess uterus, notify health care provider Total volume – 240 – 270 ml Resume menstrual cycle within 6 – 8 weeks, breast feeding may be 3 months Episiotomy, Lacerations, C/S Incisions Inspect the perineum for episiotomy/lacerations with REEDA assessment Inspect C/S abdominal incisions for REEDA R = redness (erythema) E = edema E = ecchymosis D = drainage, discharge A = approximation Postpartum Nursing Interventions Relief of Perineal Discomfort Ice packs for 24 hours, then warm sitz bath Topical agents - Epifoam Perineal care – warm water, gently wipe dry front to back Hemorrhoids, Homan’s Sign Assess for hemorrhoids Relief of hemorrhoidal discomfort may include Sitz baths Topical anesthetic ointments Rectal suppositories Witch hazel pads - Tucks Extremities Assess for pedal edema, redness, and warmth Check Homan's sign – dorsiflex foot with knee slightly bent FIGURE 23–9 Homans’ sign: With the woman’s knee flexed, the nurse dorsiflexes the foot. Pain in the foot or leg is a positive Homans’ sign. Emotional Status/Bonding Assessment Describe level of attachment to infant Determine mother's phase of adjustment to parenting Postpartum Blues Transient period of depression Occurs first few days after delivery Mother may experience tearfulness, anorexia, difficulty sleeping, feeling of letdown Usually resolves in 10 to 14 days Causes: Changing hormone levels, fatigue, discomfort, overstimulation Psychologic adjustments Unsupportive environment, insecurity Postpartum Nursing Interventions After pains Uterine contractions as uterus involutes Relief of after pains Positioning (prone position) Analgesia administered an hour before breastfeeding Encourage early ambulation - monitor for dizziness and weakness Medications Bleeding oxytocin (Pitocin) – watch for fluid overload and hypertension methylergonovine (Methergine) – causes hypertension prostaglandin F (Hemabate, carboprost) – n/v, diarrhea Pain Medications NSAIDS – GI upset Oxycodone/acetaminophen (Percocet) – dizziness, sleepiness PCA – Morphine for C/S – respiratory distress docusate (Senna) – causes diarrhea Rubella Vaccine – titer 1:10, do NOT get pregnant for 3 months Rh Immune Globulin (RhoGAM) – Rh negative mother – do not administer rubella vaccine for 3 months Mother and Family Needs Nurse can assist in restoration of physical well- being by Assessing elimination patterns Determining mother's need for sleep and rest Encourage regular diet as tolerated and increasing fluids Identify available support persons - involve support person and siblings in teaching as appropriate Determine family's knowledge of normal postpartum care and newborn care Breastfeeding Pathophysiology Before delivery, increased estrogen stimulates duct formation, progesterone promotes development of lobules and alveoli After delivery, estrogen and progesterone decrease, prolactin increases to promote milk production by stimulating alveoli Newborn suck releases oxytocin to stimulate letdown reflex Composition of Breast Milk Breast milk is 90% water; 10% solids consisting of carbohydrates, proteins, fats, minerals and vitamins Composition can vary according to gestational age and stage of lactation Helps meet changing needs of baby Foremilk – high water content, vitamins, protein Hindmilk - higher fat content Immunologic and Nutritional Properties Secretory IgA, immunoglobulin found in colostrum and breast milk, has antiviral, antibacterial, antigenic-inhibiting properties Contains enzymes and leukocytes that protect against pathogens Composed of lactose, lipids, polyunsaturated fatty acids, amino acids, especially taurine Cholesterol, long-chain polyunsaturated fatty acids, and balance of amino acids in breast milk help with myelination and neurologic development Advantages of Breastfeeding Provides immunologic protection Infants digest and absorb component of breast milk easier Provides more vitamins to infant if mother's diet is adequate Strengthens mother-infant attachment No additional cost Breast milk requires no preparation AAP= Only food for 6 months, w/ foods for 12 months Breastfeeding Mother Breastfeeding mother needs to know How breast milk is produced How to correctly position infant for feeding Procedures for feeding infant Number of times per day breastfed infant should be put to the breast How to express and store breast milk How and when to supplement with formula How to care for breasts Medications that pass through breast milk Support groups for breastfeeding Review signs and symptoms of engorgement, plugged milk ducts, mastitis Breastfeeding Assessment Figure 29–2 Four common breastfeeding positions. A, Football hold. B, Lying down. C, Cradling. D, Across the lap. Cesarean Section Needs Assess vital signs Assess breasts Assess location and firmness of uterine fundus Assess lochia Assess incision site – REEDA Assess breath sounds Assess indwelling urinary catheter - color and amount of urine noted Assess bowel sounds: present, hypoactive or hyperactive Cesarean Section Needs Cesarean birth is major abdominal surgery - if general anesthesia used, abdominal distension may cause discomfort, assess for bowel obstruction Position client on left side, include exercises, early ambulation, increase po intake, avoid carbonated beverages, avoid straws - may need enemas, stool softeners, antiflatulent meds Pulmonary infections may occur related to immobility and use of narcotics because of altered immune response Pain and Comfort Administer analgesics within the first 24 to 72 hours - allows woman to become more mobile and active Comfort is promoted through proper positioning, back rubs, and oral care - reduce noxious stimuli in environment Encourage visits by family and newborn, which provides distraction from painful stimuli Encourage non-pharmacologic methods of pain relief (breathing, relaxation, and distraction) - encourage rest Attachment After a Cesarean Birth Physical condition of mother and newborn and maternal reactions to stress, anesthesia, and medications may impact mother-infant attachment By second or third day, cesarean birth mother moves into "taking-hold period" Emphasize home management and encourage mother to allow others to assume housekeeping responsibilities Stress how fatigue prolongs recovery and may interfere with attachment process Discharge Instructions S/S complications Referral numbers PP Exercises Nutrition Rest PP appointment Avoid overexertion Birth certificate info Sexual activity Infant care Hygiene Infant complications Sitz baths Infant follow-up Incision care Family bonding Discharge Teaching New mother should gradually increase activities and ambulation after birth Avoid heavy lifting, excessive stair climbing, strenuous activity, vacuuming Resume light housekeeping by second week at home Delay returning to work until after 6-week postpartum examination Discharge Teaching Recommend exercise to provide health benefits to new mother Encourage patient to begin simple exercises while on nursing unit Inform her that increased lochia and pain may necessitate a change in her activity Sexual Activity and Contraception Sleep deprivation, vaginal dryness, and lack of time together may impact resumption of sexual activity Usually sexual intercourse is resumed once episiotomy has healed and lochia has stopped (about 3 – 6 weeks) Breastfeeding mother may have leakage of milk from nipples with sexual arousal due to oxytocin release Contraception Information on contraception should be part of discharge planning Nursing staff need to identify advantages, disadvantages, risk factors, any contraindications Breastfeeding mothers concerned that contraceptive method will interfere with ability to breastfeed - they should be given available options – progesterone only Parent-Infant Attachment Tell parents it is normal to have both positive and negative feelings about parenthood Stress uniqueness of each infant Provide time and privacy for the new family Include parents in nursing intervention Infant Care New mother and family should know basic infant care Information about tub baths Cord treatment, When to anticipate cord will fall off Family should be comfortable in feeding and handling infant, as well as safety concerns Immunizations When to call the doctor Discharge Teaching Nurse should review with new mother any information she has received regarding postpartum exercises, prevent of fatigue, sitz bath and perineal care, etc. - nurse should spend time with parent to determine if they have any lastminute questions before discharge Printed information about local agencies and support groups should be given to new family Types of Follow-Up Care Telephone calls - listen carefully and ask open-ended questions Return visits - Within one week after first visit Telephone follow-up - Within 3 days of discharge Baby care/postpartum classes New mother support groups Need to have a caring attitude in these activities