Normal Postpartum
advertisement

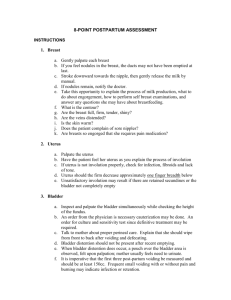
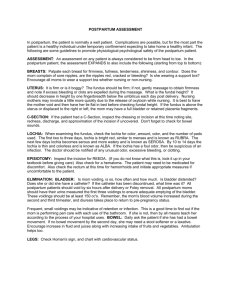
Chapter 21 Normal Puerperium It is the period of recovery that occurs from childbirth and extends for 6 weeks after delivery What is involution? Reproductive System Changes The Uterus What are the three ways that the uterus involutes? Contraction of the Uterus Muscle fibers become shorter controlling the bleeding by compressing and sealing off blood vessels – Acting as “the living ligature” Protein Material Catabolism Release of a proteolytic enzyme into the endometrium and myometrium. This enzyme breaks down the protein material in the hypertrophied cells causing the uterine muscle cells to decrease in size The uterus gradually decreases in size as the cells grow smaller Regeneration of the Endometrium – the placenta site heals in about 6 weeks with the other part healing in 3 weeks. – Heals by exfoliation rather than by forming scar tissue. – The endometrium grows from the margins of the placental site and from the fundi of the endometrial glands left in the basal layer of the placental site Critical Thinking Why does the uterus heal by Exfoliation and not by primary intention? Uterine Changes Placement and size – Where is the normal placement of the uterus immediately after birth, 12 hours later? – What is the size of the uterus? Uterus What nursing intervention should the nurse encourage PRIOR to assessing the fundus? Uterine Changes What What is the normal tone of the uterus? is the technique used to assess the uterus? Uterine Involution What is the PRIORITY intervention when the uterus is found to be boggy? Why is it important not to over-stimulate the uterus? Uterus What interventions must the nurse include if the uterus is found deviated from midline? Short Answers The nurse is going to assess the uterus. The 3 main assessments include: 1. 2. 3. The normal height of a first day postpartum woman is ________________. It should decrease _____fingerbreadth per _______. The tone should be __________. If found boggy, the nurse would ___________ the uterus. Lochia What are the three types of lochia? What is a normal amount? What question is important to ask the woman when assessing amount? What is normal odor of Lochia? Characteristics of Lochia Should not be excessive in amount Should never have an offensive odor Should not contain large pieces of tissue Should not be absent during the first 3 weeks Should proceed from rubra -- serosa -- alba Match the Lochia Lochia rubra Lochia serosa Lochia alba A. Pinkish serum with mucus and debris usually occurs on day 3 - 10. B. Creamy yellowish brownish. Occurs after day 10 C. Dark Red and consists mainly of blood. Occurs day 1 - 3. Fill in the Blank Lochia should never be ______________ in amount. Lochia should never have an ______________odor. Lochia should not contain __________ _________ of tissue Lochia should not be _____________ during the first ________ weeks Lochia should proceed from _________ to _________ to ___________. Cervix Remains soft and flabby, appears bruised and may have some lacerations No longer does the external os have the pre-pregnant appearance -- now appears as a jagged slit not a circle. Vagina May be edematous and bruised. Rugae begin to appear when ovarian function returns. May teach the mom to do Kegels exercises to increase the blood flow to the area and aid in healing Perineum Assess: the episiotomy the same as with any incision. – – – – – R – redness E – edema or swelling E – ecchymosis or bruising D – drainage A – approximated How should the nurse assess the perineum? What are measures to teach the mom in caring for the perineum? Comfort Measures Relief – – – – of Perineal Discomfort Ice packs Topical agents Perineal care Sitz bath Relief of hemorrhoidal discomfort may include – Sitz baths – Topical anesthetic ointments – Witch hazel pads Ovulation and Menstruation When does Menstruation generally return? Return is prolonged for the breastfeeding mom because of alterations in the gonadotropin-releasing hormone production. Ovulation and Menstruation Nurses need to teach moms that breastfeeding is NOT a reliable means of contraception. WHY Breasts Allow the mother to assess her own breasts -similar to doing a self-breast exam – ask if feels any nodules, lumps – ask if nipples are sore, reddened, blisters, cracks – Assess nipples for everted, flat, inverted Teach to care for breasts according to whether they are breastfeeding or bottle feeding. Process of Lactation Sucking of infant stimulates the nerves beneath skin of the areola to transmit messages to the hypothalamus Hypothalamus sends messages to the pituitary gland – Anterior pituitary -- stimulates Prolactin to be released which is the ultimate stimulation for milk production – Posterior pituitary -- releases Oxytocin which stimulates the contraction of the cells around the alveoli in the mammary glands. This causes milk to be propelled through the duct system to the infant. This is the “LET-DOWN” reflex. Felt as a tingling sensation Breastfeeding Care No soap on the nipples, wash in water wear supportive bra Breastfeeding tips: – Most important is the “latch-on” Teach measures to assist with the infant getting the nipple and areola in the mouth – Teach different positions to hold the baby – No timing – Relax to allow for “let-down” – express colostrum on the nipples after feeding – remember drops of colostrum are the same as ounces of milk -- if wetting 6 - 10 diapers / day, then must be getting enough to eat Suppression of Lactation Key is to teach the mother measures to decrease stimulation of the breasts – Wear a tight-fitting bra or binder – Do not express milk from the breasts – Take shower with back to the warm water – Ice packs Fill in the Blank The Anterior pituitary stimulates the release of ___________________ which is responsible for _________ _____________________. The posterior pituitary gland releases ___________ which is responsible for the ______-__________ reflex. Short Answers What are four important interventions to teach a mom who is bottle feeding to decrease stimulation of the breasts. 1. 2. 3. 4. Cardiovascular System Changes How does the body rid itself of excess Plasma volume? Blood Volume – Increase for about 24-48 hours after delivery – Increase in blood flow back to the heart when blood from the placenta unit returns to central circulation – Extravascular interstitial fluid is moved into the vascular system / intravascular – Leads to increased cardiac output mainly RT increase stroke volume. Blood Values Pregnancy Post Partum WBC – elevated slightly to about 12,000 WBC – leukocytosis is common with values of 25,000 – 30,000 RT increased neutrophils RBC – increase slightly to about 10 milion. RBC – return to normal Hemoglobin – stays about normal at ~ 12 g. Below 10 g = anemia Hemotocrit – lowers 33-39% RT hemodilution. If drops below 3235% = anemia Hgb. – normal to see a drop of about 1 gram Hct – normal to see a drop of about 2- 4 points and then a rise RT > loss of plasma than RBC death Platelets – drop and gradually rise Assess for Thromboembolism – During pregnancy, plasma fibrinogen (coagulation) increases, Mother’s body has the ability to form clots and prevent excessive bleeding. – Plasminogen (lysis of clots) does not rise – Hypercoagulable state and the woman is at a greater risk for thrombus formation. – assess for homan’s sign Vital Signs Temperature – A slight elevation of up to 100.40 may occur related to dehydration and increase basal body metabolism from exertion of labor and delivery. – After 24 hours, the temperature should be normal – A temperature greater than 100.40 suggests infection. Blood Pressure – Should remain stable – Hypovolemia can indicate postpartum hemorrhage – Hypervolemia could indicate preeclampsia Vital Signs Pulse – Bradycardia of 50 – 70 bpm is Normal – Tachcardia is not considered a normal occurrence and may indicate excessive blood loss Respirations – Should remain stable and within normal range Critical Thinking The woman’s vital signs are: T.100.8, P- 56, R – 16, B/P – 110/65. How would the nurse interpret these findings? What interventions are indicated? Gastrointestinal Tract The most common GI problem during postpartum is constipation – EXPLAIN. What teaching is important to assist in decreasing constipation? Urinary System What is the most common problem associated with the urinary system? Why be concerned? Critical Thinking A primigravida delivered 2 hours ago. The woman states she would like to go to the bathroom. What should the nurse do? The woman is unable to void. What should the nurse do next? Afterpains Who is more likely to experience afterbirth pains? Explain. Relief of after pains – Positioning (prone position) – Analgesia administered an hour before breastfeeding – Encourage early ambulation - monitor for dizziness and weakness Rest and Activity Most common problem is Sleep -- the excitement and exhilaration experienced by birth my make it difficult to sleep. They are tired and need rest. Allow for times of uninterrupted sleep. Exercises -- have the patient to ask her own doctor for specific exercises. Usually walking is safe. May eventually do postpartum exercises. Just need to allow the body to return to its prepregnant state before straining it. Resumption of Activities New mother should gradually increase activities and ambulation after birth She should avoid heavy lifting, excessive stair climbing, strenuous activity Resume light housekeeping by second week at home Delay returning to work until after 6-week postpartum examination Exercises Recommend exercise to provide health benefits to new mother Nurse should encourage client to begin simple exercises while on nursing unit Inform her that increased lochia and pain may necessitate a change in her activity Pain Perineal pain -- caused from trauma during delivery, episiotomy, hemorrhoids. Provide comfort measures such as: sitz baths, Tucks, Sprays / Foams, oral analgesics. Afterbirth pain -- more common in multigravidas and breastfeeding moms. Treat with * mild analgesics (NSAIDS, Acetamenaphen),heating pad, lie on abdomen, discontinue use of oxytocins, Breast engorgement -- warm or cold packs, increase feedings, decrease stimulation. Bind breasts. Gas distention -- no ice, increase warm / hot fluids, increase walking, rocking chair, antiflatus drugs. Decision Making During shift assessment of the post partum mom’s peri pad, the nurse found it saturated with lochia rubra. What would be the priority nursing intervention? The Nutrition Need Most moms are hungry and eager to eat. Start off slowly to avoid nausea and vomiting. Diet should include: – High in Protein, vitamin C, and fiber – Increase in fluids Lactating moms need about 700 extra calories for milk production Prenatal vitamins and iron supplements are often continued in the postpartum period. Psychological Adjustment The responses of the mother to the birth of her infant are influenced by many factors such as: – Her parents own birth -- parenting and nurturing – Cultural background -- only by understanding and respecting the values and beliefs of each woman can the nurse plan and meet the patient’s needs – Readiness for parenthood -- emotional maturity, pregnancy planned or unplanned, financial status, job status – Freedom from discomfort -- physical condition – Health of her newborn -- physical condition, prematurity, congenital defects – Opportunities for parent- infant interactions Postpartum Blues Transient period of depression – Occurs first few days after delivery – Mother may experience tearfulness, anorexia, difficulty sleeping, feeling of letdown Usually resolves in 10 to 14 days Bonding Initial attraction felt by parents Contact should occur as early as possible and as frequently as possible. Allow time for attachment to occur with all members of the family Attachment Bond that endures over time Occurs through mutually satisfying experiences Reciprocity - Mutually gratifying interaction among mother, infant, father Attachment Process Enface - infants face on same vertical plane as parent. Mutual gazing Explore with finger-tips Hand and Palmar contact Whole arms --enfolds whole baby close to body Claiming The Claiming Process Includes the identification Of the baby’s specific Features, relating them To other family members “Those long toes are just like his Dad’s” The Steps in Attachment are: 1. 2. 3. 4. Postpartum Phases by Rubin Taking - in – Occurs during day 1 - 3 following delivery. – Marked by a period of being dependent and passive behavior. – Mother’s primary needs are her own -- food and sleep – Mother is talkative about her labor and delivery experience ***Main nursing is to listen and help the mother interpret events of the delivery to make them more meaningful and clarify and misconceptions Postpartum Phases by Rubin Taking - Hold – Occurs during day 3 to about 2 weeks postpartum – Ready to deal with the present – More in control . Begins to take hold of the task of “mothering” ***It is the best time for teaching! Tailoring teaching to individual Learning Styles – Demonstrations – Group Classes – Videotapes Postpartum Phases by Rubin Letting Go Phase – occurs after about 2 weeks – Mother may feel a deep loss over the separation of the baby from part of her body and may grieve over this loss. – Common for Postpartum Blues to occur during this time Father-Infant Interaction Engrossment – Sense of absorption – Preoccupation Interest in infant Discharge Preparation for discharge should begin when expectant mother enters birthing unit Mother needs to be aware of signs of postpartum complications and should be aware of her self-care needs Nurses should begin first by assessing knowledge and expectations of new mother and family Nurse should be available to answer questions and provide support to parents Discharge Printed Information Nurse should review with new mother any information she has received regarding postpartum exercises, prevent of fatigue, sitz bath and perineal care, etc. - nurse should spend time with parent to determine if they have any last-minute questions before discharge Printed information about local agencies and support groups should be given to new family The End