C-Section Patient Teaching
advertisement

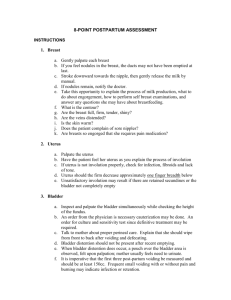
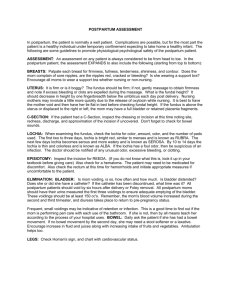
OB Nursing The Postpartum Period Learning Objectives • At the end of this lesson, the student nurse will be able to: • 1. Discuss physical changes that occur during the postpartum period • 2. Discuss psychosocial changes that occur during the postpartum period, including adjustment to parenting • 3. Describe the role of the nurse in postpartum care • 4. Describe what is necessary to teach mom during the postpartum period Review Stage 4 of Labor and Delivery • Immediately after delivery: • Major concern is hemorrhage • VS every 15 minutes until stable • Check uterine fundus for firmness and position (I will discuss this in more detail) • Check perineum for REEDA • Check peri-pad for vaginal discharge • Ice to perineum to reduce edema and discomfort • Stage lasts1-2 hours or until mom is stable Postpartum Period- NSVD • First 6 weeks after delivery • This is the time when the reproductive organs return to their nonpregnant state Physiologic Changes in Reproductive Organs • UTERUS • • • • The shrinking of the uterus to the non-pregnant size is called involution After delivery, the uterus is the size of a grapefruit It is at the level of the umbilicus a few hours after birth **Each day it descends approximately 1 fingerbreadth lower in the abdomen until the 10th day when it can no longer be felt because it is back in the pelvic cavity Uterus Con’t. • Mild uterine contractions called “afterpains” as the uterus contracts to control bleeding • IMPORTANT for mom to void every 2-3 hours. A full bladder will interfere with uterine involution and bleeding will be increased!!! Vaginal Discharge After Delivery • Vaginal discharge after delivery is known as lochia • Lochia is due to the sloughing of the uterine layer where the placenta was attached • Lochia contains blood, mucus, tissue, WBC’s, and bacteria 3 Stages of Lochia • 1.Lochia Rubra- 1st 3 days postpartum. Is bright red and resembles a menstrual period. Moderate amount and has a menstrual flow odor • 2. Lochia Serosa- 4 to 10 days. Is brownish, pinkish brown. Small to moderate amount. • 3. Lochia Alba-Around the 11th-21st day. Yellowish white. Small to moderate amount. May continue for a few weeks Lochia Facts • There is a decreased amount in c-sections because the uterus is suctioned after delivery • There is an increase in lochia flow when ambulating for the FIRST time because of pooling in the vagina • A foul odor is ABNORMAL! • The progression of lochia through the 3 stages is important because it indicates normal uterine healing • Menstrual Period• Returns in bottle feeding moms usually within 2-3 months after delivery • Returns in breastfeeding moms by 6 months or when lactation ends Lochia-Patient Teaching • Explain to mom what to expect day by day in lochial flow • Instruct mom to change peri pad every 2-3 hours and with every voiding • Instruct on the correct technique- touch the outside edges of the pad only and apply from front to back • Clean peri area after each voiding with peri bottle or wand faucet • Instruct mom to call the physician for any foul odor, increased flow, or bloody flow after 5 days Postpartum VS • Vital Signs-every 4 hours for the first 24 hours and then BID • Temp- up to 100.4 is considered NORMAL! • Temp may be slightly elevated due to blood loss or dehydration • If the temp is above 100.4, this warrants further assessment • Pulse: generally bradycardia- 50-70 bpm. Pulse returns to normal in 1 week due to a reduction in blood volume Postpartum VS Con’t. • A rapid pulse indicates hemorrhage, infection or anxiety • BP remains stable or slightly lower due to blood/ fluid loss • Respirations: slower and less labored due to absence of uterine pressure on diaphragm Postpartum Assessment • BUBBLE • • • • • • BREASTS UTERUS (FUNDUS) BLADDER BOWEL LOCHIA EPISIOTOMY BREAST ASSESSMENT • Secrete colostrum at the end of pregnancy which is high in antibodies and protein • After 2-3 days breast milk is secreted • Breasts become firm and tender as breast milk accumulates • If mom breast feeds, the breasts will fill and empty as needed • The act of breast feeding stimulates milk production • If mom bottle feeds, the breasts will fill with milk a few days after delivery and will be firm and tender • Without stimulation this milk will be reabsorbed and the breasts return to normal in 2-3 days Breast Assessment Con’t. • The breasts are palpated for softness, firmness, tenderness, engorgement (very firm and painful R/T milk accumulation) • Nipples are checked for cracking, sores, inversion(nipples turn inward) Breast Care • Prolactin and oxytocin control milk production and ejection • Infant sucking on the breasts stimulates milk production • At 1st, the infant should nurse for 2-5 minutes on each breast every 23 hours • Frequent feeding stimulates the production of more milk • If the breasts are not stimulated, milk production stops Patient Teaching- Breast Care • Colostrum can be rubbed onto nipples to prevent drying • Lanolin can be applied to nipples for soreness • Air dry nipples for 15 minutes TID • NO soap to breasts. Mom should wear a supportive bra AAT!!!! • Feeding positions- cradle, football, side lying • How to latch on and how to remove newborn from the breast • Mark the breast with a pin for the next feeding Breast Engorgement (days 3-5) • Can occur in breastfeeding and bottle feeding moms • Breast become hard, firm and tender as they fill with breast milk • In bottle feeding moms, it lasts a few days and then milk production ceases • Comfort measures include a supportive bra or binder, ice packs, and analgesics • To relieve breast engorgement in breastfeeding moms, FEED the baby! Uterus Assessment • The fundus is palpated for position (fingerbreadths below the umbilicus) • The fundus should be midline of abdomen-NOT to the side ( indicates a full bladder) • Should be firm like a grapefruit- soft or “boggy” uterus puts mom at risk for bleeding Bladder Assessment • Check with mom to be sure she is voiding sufficiently and at least every 2-3 hours • There is diuresis after delivery • Urinary output may reach 3000 ml within 24 hours • It is important for mom to void within 6-8 hours to prevent hemorrhage • Should void at least 150-200 ml of clear yellow urine per voiding • Mom may not be aware of the need to void due to trauma during L&D or anesthesia Bladder Assessment Con’t. • A distended bladder pushes the uterus upward and to the side • A distended bladder will interfere with uterine involution, cause increased pain and can lead to infection and hemorrhage • If unable to void, a Foley catheter will be placed • Patient Teaching –Urinary Elimination• Increase fluid intake • Void every 2-3 hours • S/S of bladder distention and retention-voiding in small amounts, change in abdominal contour, fundus is shifted to the side, increase in lochia rubra (uterus can’t contract correctly) Bowel Function Assessmnet • Bowel function will be slow due to hormones • Mom may fear defecation due to pain in the area • Stool softeners, laxatives and topical preparations relieve pain • Dulcolax suppositories are ordered PRN as well as enemas • C-section patients, bowel sounds should be assessed every shift, check for flatus • Patient Teaching• Fluids, Ambulation, Fiber intake Lochia Assessment • Assess for color, amount, odor, and presence of clots • Teaching has already been discussed Episiotomy Assessment • Assessed for REEDA • Redness or inflammation • Ecchymosis • Edema • Discharge (from incision) • Approximation of suture line • **The anus is assessed at the same time for hemorrhoids Patient Teaching- Episiotomy • Sitz baths or peri bottle to cleanse the area and promote healing • Pain meds • Dermoplast spray Pain Level- Postpartum • Assess pain every 4 hrs. • Medicate before pain is out of control • Patient Teaching regarding Pain• • • • • • • • Ice packs to perineum for 1st 24 hours Sitz baths tid after 12-18 hours Contract buttocks when sitting Donuts to sit on Peri bottle with warm ater after voiding Tucks, dermoplast, proctofoam, pain meds Instruct patient in meds she has ordered and how often she can be medicated Mom will self medicate on the unit Assessment of Lower Extremities • Assessing the mother’s extremities to check for thrombophlebitis • There is an increase in clotting factors during pregnancy • Legs are checked for redness, temperature changes, shape, symmetry and edema • Positive Homan’s sign indicative of thrombophlebitis • Patient Teaching• Don’t cross legs • Ambulate, exercise Assessment of Hemorrhoids • • • • • • • • • Assess their presence and whether or not they are bothersome to Mom Distended blood vessels in anus, internal, external May disappear in weeks following delivery Patient TeachingWarm sitz baths, cold compresses, Tucks, Proctofoam HC spray are helpfulPAIN MEDS Increased fluids and fiber are encouraged to prevent constipation Rubber donuts for sitting Ask c-section moms if they are bothered by hemorrhoids from pregnancy Contract buttocks Routine Assessment for C-Sections • This includes abdominal post-op assessment as well as PP assessment • Assess: • VS q4h x 48-72 hours • Incision, dressing, staples, incision for S&S of infection, dehiscence, evisceration • Bowel sounds-active, hypo, hyper • Passing flatus • Distention-hard or soft • Breath sounds • IV site for S&S of infection • Voiding-will have foley for 1st several hours C-Section Assessment Con’t. • Breasts • Position and consistency of fundus • Lochial flow • Perineum should be intact • C-Section Patient Teaching • Ambulation will stimulate BS to return, prevent DVT and repiratory problems • Increased fluids will prevent UTI and constipation • Avoid carbonated drinks- will cause gas C-Section Patient Education Con’t. • S&S of infection-redness, drainage from incision, dehiscence, increased pain • Pain meds-what’s ordered and how much • When to call MD Other Patient Teaching in the PP Period • Baby care(will discuss later) • When to contact MD: fever > 100.5, loss of appetite, change in activity, vomiting, diarrhea, extreme irritability • No intercourse or tampons for 6 weeks after delivery • Rest several times a day • Do not lift anything heavier than baby PP Lab Work • Average blood loss during delivery is approx. 250-500 mL. • Normal woman can tolerate this blood loss without difficulties • H&H return to normal 1 week after delivery • WBC is elevated due to stress of delivery and healing of placental site • Patients will have an H&H drawn the 1st PP day • PNV and Fe supplements may be ordered if indicated Postpartum Psych Changes • Mom very self centered, relives birthing experience over and over • After delivery often dependent on others for her care • Often has mood swings R/T discomfort, fatigue, and hormone changes • Some experience “PP blues” or “baby blues” about day 3 days postpartum and is evidenced by: irritability, poor appetite, insomnia, tearfulness, crying-this is a temporary situation PP Psych Changes- Depression • Is a nonpsychotic depressive illness and is usually manifested within 4 weeks after delivery • Stresses experienced at this time by Mom include: • • • • • • Physical changes, discomfort, concern about figure Changing family relationships Emotional stress, feeling of being tied down Lack of time for her personal needs and interests Loss of concentration Intense feelings of inadequacy, guilt, inability to cope PP Depression • Treatment • • • • • • Psychotherapy Antidepressant medications Phototherapy as well as exercise are complimentary treatment strategies Hormonal skin patches Family counseling Follow-up with a case manager or therapist Postpartum Psych Changes- Psychosis • Have an impaired sense of reality • A woman may have any psychiatric disorder • Can be fatal for both mother and baby • Mom has poor judgment, has a sense of being vulnerable • Suicide and infanticide are possible • Rx- outpatient or inpatient psychiatric counseling depending on the severity. Psychotropic meds. Breastfeeding is contraindicated while on these meds. Drugs Used in the Postpartum Period • Class- serum immune globulin • Drug- RhoGam, Rho (D) Immune Globulin • Action- prevents the production of anti-Rh antibodies in Rh- people, and therefore prevents hemolytic disease in Rh+ newborn • Route- IM. Administered at 28 weeks gestation and within 72 hours of delivery, also administered after amniocentesis, miscarriage, abortion, ectopic pregnancy • Contraindications- Rh+ patients • Side Effects-painful injection site, fever • Nursing- Educate patient in purpose of the drug Drugs Con’t. • Dermoblast- benzocaine 8% and menthol • Topical anesthetic and antipruritic for relief of skin pain and itching due to abrasions, burns, skin irritations • Side Effects-rash, increased irritation Drugs Con’t. • Proctofoam-hydrocortisone 1%, pramoxine HCL 1% • Topical corticosteroid used for inflammation and pruritic manifestations and dermatosis of anal region • DO NOT INSERT INTO ANUS!!! • Adverse Reactions- burning, itching, irritation, dryness, hypopigmentation, acneform eruptions, striae, skin atrophy, secondary infections maceration Drugs Con’t. • PNV- Prenatal Vitamins • Vitamins-A, D, E, C, folic acid, thiamine, riboflavin, niacinanmide, B6, B12 • Minerals- calcium, copper, iron, zinc • Indications- vitamin and mineral supplement throughout pregnancy and lactation • Dosage- one tablet daily • Side Effects- rare, epigastric distress sometimes occurs when administered on an empty stomach, administer with meals, citrus juice enhances absorption