Post_Fossa_Tumors PPT Slides
advertisement
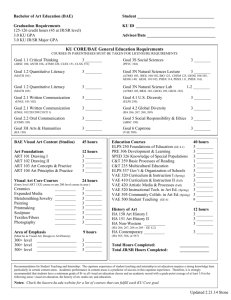
Posterior Fossa Procedures (Infratentorial Craniotomy) and Neuroanesthesia Emergencies Mani K.C Vindhya M.D Asst Prof of Anesthesiology Nova Southeastern University Anesthesia for Posterior Fossa Procedures (Infratentorial Craniotomy) and Neuroanesthesia Emergencies I. Format = approach to posterior fossa case Preoperative concerns – Problem list? Further labs and studies? Optimization? (Is the patient optimal for surgery?) Consults? Further medical treatment? Intraoperative concerns Premedication Monitoring Induction Maintenance Intra-op complications (2 main complications?) Emergence Postoperative concerns – only on the long stem 2 main complications? Post-op pain relief Posterior fossa considerations Case Presentation. An 18 year-old male for posterior fossa exploration and excision of cerebellar mass lesion. History headache nausea and vomiting impaired hearing occasional diplopia Physical exam ataxia severe bilateral papilledema (3/4) BP = 120/70 to 140/80 weight = 65 kg CT scan cerebellar mass lesion hydrocephalus The neurosurgeon desires intraoperative monitoring of: brain stem auditory evoked potentials (BAEP's) facial nerve (cranial nerve VII) function Problem List: Cerebellar mass lesion with hydrocephalus Increased ICP Positioning -- sitting, prone, lateral, or supine (semi-lateral) "Full stomach" -- nausea and vomiting, increased ICP Intraoperative monitoring Brainstem auditory evoked potentials Facial nerve function (motor testing) Posterior Fossa Is a "closed-in" space Bone - on sides, back, and bottom Tentorium - on top (Posterior fossa is "infratentorial.") Brain stem - in front Contains about 1/4 of intracranial contents Tumors in the posterior fossa Children Intracranial neoplasms = the most common solid tumors in childhood (about 25% of all admissions for neoplastic disease). Posterior fossa = the site of origin of 50 to 60% of brain tumors in children. Adults -- uncommon site for brain tumors Tumors in the posterior fossa are often: "Benign by histology" "Malignant by location" Posterior fossa tumors can compress the brain stem (pons and medulla). CSF outflow tracts Cardiovascular centers Respiratory centers -- pneumotaxic center, apneustic center Posterior Fossa 3 dorsal respiratory group, ventral respiratory group d. Lower cranial nerves (and functions): V Trigeminal Facial sensation VI Abducens Eye abduction VII Facial Facial muscles (motor) VIII Acoustic Hearing IX Glossopharyngeal Gag reflex X Vagus Cough reflex, laryngeal muscles XI Spinal accessory Shoulder movement XII Hypoglossal Tongue movement Explanation of symptoms in case presentation - 1. Elevated intracranial pressure (ICP) triad secondary to hydrocephalus headache, nausea (and vomiting), papil edema 2. Cerebellar involvement -- ataxia 3. Brain stem involvment a. Hearing loss (involvement of C.N. VII ) b. Diplopia (probably involvement of C.N. VI) Sitting Position Situations in which sitting position might be used are mainly: Posterior fossa procedures Cervical laminectomy Establish which position the surgeon desires for posterior fossa surgery: Sitting Prone Lateral decubitus Supine (semi-lateral) Proper positioning for a seated posterior fossa operation Knees at heart level Neck not hyperflexed Sitting Position Advantages of the sitting position include: Excellent surgical access Comfort for the surgeon Facilitates hemostasis (decreased blood loss) Improved venous and CSF drainage Exposes face for monitoring response to cranial nerve stimulation (though this can also be done electronically) Possible sitting position complications include: Air embolism (venous and arterial) Cardiovascular instability Hypotension Venous pooling Cardiac arrhythmias Neurologic complications Quadriplegia Nerve injuries (e.g. ulnar, sciatic, lateral peroneal) Pneumocephalus Airway obstruction Airway swelling (head and tongue) Malpractice risk. The use of the sitting position for posterior fossa neurosurgery is somewhat controversial. Current practice is away from operating in sitting position6 No evidence that position affects outcome. Venous air emboli can occur in any position -sitting, lateral, prone, or supine Relative Contraindications to Sitting Position Known cardiac septal defect = a "red flag" Patent foramen ovale (PFO) Atrial septal defect Ventricular septal defect Right atrial pressure > left atrial pressure Functioning ventriculo-atrial shunt ?? cardiac instability ?? extremes of age Air Emboli (Venous and Arterial) Incidence of venous air emboli (VAE) can be as high as 50% in neurosurgery. Incidence of VAE depends on both monitoring and position.10 "Bottom line" on VAE: More frequent in the sitting position. BUT -- VAE can occur in any position. Early detection and prevention with the Doppler and other more sensitive VAE monitoring methods have: Decreased the occurrence of clinically significant VAE Increased the reported incidence of VAE Relative sensitivity of techniques to monitor for VAE Comments on VAE monitors Bubble Doppler -- still a very sensitive and practical way to detect VAE Transesophageal ECHO (TEE) The most sensitive way to detect VAE. The only way to document intraoperative "paradoxical air emboli" which have crossed to the arterial circulation, unless the surgeon sees air bubbles in arteries! ECHO could be used to detect a patent foramen ovale preop. Incidence of patent foramen ovale = about 1 in 4. A paradoxical air embolus can occur even if a person does not have a patent foramen ovale. Air can traverse the pulmonary circulation. Why don't we get pre-op ECHO's for all sitting position cases? Expensive The number of complications as a result of paradoxical air emboli is actually small Pulmonary artery pressures (PAP) CVP catheters: Have two uses regarding VAE: VAE detection (much less sensitive than Doppler or TEE) VAE aspiration (potentially life-saving in some situations) How do you confirm CVP catheter placement in the right atrium (to aspirate air lock if VAE occurs)? Length of catheter (but could be in jugular vein) Rapid saline bolus through CVP (listen to Doppler) PAC's (imply atrial stimulation) PVC's (imply ventricular stimulation) Right ventricular pressure wave on CVP (Pull catheter back into right atrium.) Chest X-ray Biphasic P-wave on intracardiac electrocardiogram Biphasic P-wave on intracardiac electrocardiogram Intraoperative Concerns Premedication? Thorough pre-op interview to allay anxiety. None ("light" sedation with benzodiazepine if at all). Avoid narcotics pre-op (respiratory depression, nausea and vomiting). Monitoring Checklist -- use "routine" monitors as reminders: Stethoscope -- esophageal Precordial Doppler -- to detect venous air emboli (VAE) EKG -- ST segments Non-invasive blood pressure Radial A-line -- BP, paO2, paCO2 (=25-30), H&H, K+ CVP -- follow volume status, aspirate VAE Temperature -- esophageal probe Blood warmer, Bird or Bear humidifer Warming/cooling blanket Oxygen monitor (+ volume monitor and PIP) Adjust ventilation according to paCO2 Pulse oximeter End-tidal CO2 (and infrared gas analyzer) Useful to trend paCO2 (End-tidal CO2 < paCO2) Detecting VAE (decreased end-tidal CO2, increased ET N2) Restraints (+ twitch monitor -- muscle relaxants) Intake and output Foley catheter (furosemide, mannitol) Maintain even I&O (Don't "run em' dry.") Avoid dextrose-containing solutions in IV's Position injuries Ulnar or sciatic nerves (in sitting position) Neck not hyper-flexed or -extended Special monitors 1. Facial nerve (C.N. VII) function Neurosurgeon directly stimulates facial nerve in operative field. Facial muscle movement is observed: Directly by the anesthesiologist (under drapes) Indirectly by electrode and monitor Anesthetic implication -- neuromuscular blockade must wear off or be reversed at time of stimulation. 2. Brainstem auditory evoked potentials or responses (BAEP's or BAER’s) Specialized form of EEG monitoring Background EEG activity is electronically subtracted out. The EEG waveform evoked by auditory stimulus (clicking in ear) remains. Shape of a typical BAEP = seven peaks1 – Latency = time to first peak (usually 2 msec) – Amplitude = height of the peaks c. The seven peaks of the BAEP are believed to correspond to passage of a stimulus through "generators" in the auditory nerve, brainstem and cortex. The seven peaks of the BAEP WAVE PURPORTED GENERATOR I Extracranial auditory nerve II Intracranial auditory nerve and/or cochlear nucleus III Superior olive IV Lateral lemniscus V Inferior colliculus VI Thalamus VII Thalamocortical radiation BAEP What do we look for during surgery? Mainly two things: Increase in latency (> 10%) Decrease in amplitude (<50%) These two changes could be indicative of impending injury or ischemia in the BAEP pathway. BAER's are barely affected by anesthetics: No anesthetic drug produces a change in BAER’s that could be mistaken for a surgically induced change. 2) Etomidate decreases amplitude and increases latency (but this is not clinically significant). Induction -- "typical" anesthetic regimen for intracranial procedures, assuming airway meets good criteria (i.e. Mallampati classification): 1. Method: "Modified" rapid sequence induction and intubation (with cricoid pressure) Preoxygenate and denitrogenate (100% O2 by mask with head in good "sniffing" position) Cricoid pressure (N&V with increased ICP) Hyperventilate to decrease paCO2 prior to intubation Typical induction agents Propofol, etomidate, or thiopental suitable I.V. induction agents Fentanyl or sufentanil – as narcotic analgesics to supplement Lidocaine IV – to blunt hypertensive and ICP response to intubation d. Neuromuscular junction blockers –rocuronium, vecuronium, or succinylcholine (with prior defasciculating dose of non-depolarizing NMJ blocker) Maintenance 1. Reasonable Maintenance Regimens for Intracranial Neuroanesthesia (going from routine to desperate). a. N2O + isoflurane (½%) + fentanyl N2O = the first agent to go if there’s brain swelling or venous air emboli or ischemia danger (i.e. aneurysm or head trauma) MAC equivalents of sevoflurane or desflurane might also be substituted for isoflurane. Sufentanil could be substituted for fentanyl. b. Isoflurane (1%) + fentanyl c. Isoflurane (½%) + propofol + fentanyl ! Volatile agents are next to go if high ICP or brain swelling Total IV anesthetic: Propofol + fentanyl Barbiturate coma -- for intractible brain swelling or cerebral protection during aneurysm clipping (titrated to EEG burst suppression): Thiopental Pentobarbital Non-depolarizing neuromuscular junction blocker (must wear off or be reversible by time of CN VII testing). Vecuronium Rocuronium Pancuronium – increases HR Cis-atracurium Additional maneuvers to decrease ICP Intraoperative Complications -- "Emergencies in Neuroanesthesia" Intraoperative Air Embolus What should I do immediately? Tell the surgeon, who should flood the field. Discontinue N2O and give 100% O2 Aspirate air from the CVP line Light neck compression Call for help Supportive measures (i.e., treat hypotension, arrhythmias) Try to position patient for CPR What else can I do? Other considerations: Dopamine or dobutamine? (Suggested to increase right ventricular contractility) Raise CVP by fluid loading, not PEEP. PEEP would raise CVP, but at the risk of sending a paradoxical (arterial) air embolus through a probe-patent foramen ovale. Avoid the Valsalva maneuver:This increases CVP, but: could cause paradoxical air embolus causes severe hypotension "Tight Brain" -- Think through things we can do to decrease intracranial volume and ICP. Airway disaster? In any anesthetic emergency, the first things to think of are: HYPOXIA & HYPERCARBIA! (Is this a respiratory disaster?) Furosemide and mannitol? Dexamethasone? Open the spinal drain or insert a ventriculostomy? Can I hyperventilate more (to paCO2 of 25)? Anesthetic choice? Muscle relaxant? DC N2O, switch to 100% O2? TIVA (total IV anesthetic) technique? Barbiturate coma – as a last resort Improve venous return? Reverse Trendelenberg position? Elevate head of bed? Reposition the head? Is there venous occlusion secondary to positioning? Sudden Cardiovascular Changes a. With any sudden change in vital signs (hyper- or hypotension, tachy- or bradycardia, cardiac arrhythmias, etc.), the first three things to think of in this situation are: HYPOXIA & HYPERCARBIA! (Always first) SEVERE AIR EMBOLUS (Close second) Artifact - has BP transducer or table moved up or down? b. Bradycardia 1)With hypertension a) Most likely cause = Cushing response 2ndary to: ICP (closed skull) surgical retraction (open skull) brain stem stimulation traction on trigeminal nerve (CN V) Cushing Response Potential treatments: Tell surgeon. Propofol or pentothal bolus Deepen anesthesia Other possible causes: Impending brain stem herniation (turn off spinal drain?) Inadvertent phenylephrine bolus Bradycardia With hypotension Most likely cause = vagal stimulation Potential treatments: Tell surgeon. Ephedrine Atropine (or glycopyrrolate) Tachycardia With hypertension Most likely causes = light anesthesia or sympathetic stimulation Another cause = inadvertent Ephedrine bolus Potential treatments = deepen anesthesia (1st), antihypertensives (2nd) With hypotension Most likely cause = hypovolemia Another cause = hemodynamic instability due to sitting position Potential treatments: Replace I&O cc per cc Phenylephrine Premature Ventricular Contractions (PVC's) POTENTIAL CAUSES POTENTIAL TREATMENTS ! Hypoxia Oxygen ! CVP catheter Pull back catheter in right ventricle ! Brain stem stimulation Tell surgeon ! Hypokalemia Potassium (due to diuresis) ! Hypomagnesemia Magnesium ! Intrinsic disease Lidocaine Emergence. Hypertension is frequently a problem. Avoid "coughing and bucking" while head is secured. Two agents to treat coughing and bucking are: Propofol Lidocaine It's desirable for the patient to awaken quickly so neurosurgeons can obtain a neurologic assessment. Postoperative Concerns. • Many potential postoperative problems are related to the location of the surgery on or near the brain stem. • Cardiovascular centers - hypertension • Respiratory centers - respiratory depression, apnea • Lower cranial nerves: VI VII VIII IX X Abducens Facial Acoustic Glosspharyngeal Vagus Disconjugate gaze Facial muscle paralysis Hearing loss loss of gag reflex Vocal cord paralysis