AEMT Transition - Unit 8 - Ventilation Physiology
advertisement

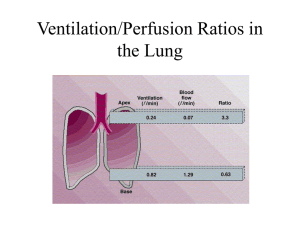
TRANSITION SERIES Topics for the Advanced EMT CHAPTER 8 Regulation of Ventilation, Ventilation/Perfusion Ratio, and Transport Objectives • Review how the body regulates normal ventilation. • Explain how feedback systems of the body can influence ventilation. • Discuss the V/Q ratio and how it influences the body. • Identify the role of red blood cells and hemoglobin in oxygen transport. Introduction • Understanding how the body ventilates and oxygenates is integral to proper care. • This chapter will look at the next several components of an organism, with focus on how ventilations are controlled and oxygen transported. Physiology • Regulation of Ventilation – Breathing is primarily involuntarily controlled – Feedback to the brain on breathing status provided by: Chemoreceptors Lung receptors Physiology (cont’d) • Regulation of Ventilation – Chemoreceptors Central chemoreceptors are located in the medulla. Monitor CO2 in arterial blood and pH of CSF. Physiology (cont’d) • Regulation of Ventilation – Chemoreceptors Peripheral chemoreceptors are located in the aortic arch and carotid bodies. More specific to changes in oxygen levels. Physiology (cont’d) • Regulation of Ventilation – Lung receptors Irritant receptors Stretch receptors J-receptors Figure 8-1 Respiration is controlled by the autonomic nervous system. Receptors within the body measure oxygen, carbon dioxide, and hydrogen ions and send signals to the brain to adjust the rate and depth of respirations. Physiology (cont’d) • Regulation of Ventilation – Hypercapnic drive The normal impetus to breathe is the level of CO2 in arterial blood. – Hypoxic drive This occurs when oxygen levels become the impetus to breathe. Physiology (cont’d) • Ventilation/Perfusion Ratio (V/Q Ratio) – Describes the relationship between the amount of ventilation and perfusion the lung receives. – Ideally the ratio would be 1, but it is not. – All etiologies of respiratory distress can be defined in terms of ventilation or perfusion deficits. Physiology (cont’d) • Ventilation/Perfusion Ratio (V/Q Ratio) – Pressure imbalances Perfusion of blood through the alveoli capillary bed can be influenced by capillary driving pressure or the air pressure within the lung. Figure 8-2 Perfusion of the pulmonary capillaries is affected by pressure within the alveoli and pressure within the capillaries. Physiology (cont’d) • Ventilation/Perfusion Ratio (V/Q Ratio) – Ventilatory disturbances Conditions that result in wasted ventilation through the lungs. The correction is to enhance alveolar ventilation. Physiology (cont’d) • Ventilation/Perfusion Ratio (V/Q Ratio) – Perfusion disturbances Conditions that result in wasted perfusion through the lungs. The correction is to enhance lung perfusion. Physiology (cont’d) • Transport of O2 and CO2 in the Blood – Oxygen transport 97%–98.5% is attached to hemoglobin 1.5%–3% is dissolved in plasma Physiology (cont’d) • Transport of O2 and CO2 in the Blood – Carbon dioxide transport 70% bound in the form of bicarbonate 23% attached to hemoglobin 7% dissolved in plasma hemoglobin and dissolved in plasma. Carbon dioxide is transported in the blood in three ways: as bicarbonate, attached to hemoglobin, and dissolved in plasma. Figure 8-3 Physiology (cont’d) • Alveolar/Capillary Gas Exchange – Gas exchange in the lungs Venous blood is low in O2 and high in CO2. Alveolar gas is high in O2 and low in CO2. When the RBC passes by the alveoli, the gases flow down their partial pressure gradients. Overview of ventilation and perfusion Case Study • You are alerted to respond to a local freeway rest stop for a patient with respiratory distress. Upon your arrival, you find the patient sitting in the lobby of the rest stop bathroom facility, looking scared. As you approach, he says to you, “I was just driving. I don‘t know what happened.” Case Study (cont’d) • Scene Size-Up – 62-year-old male patient – BSI precautions are taken – NOI is respiratory distress – There is only one patient – There are no barriers to extrication from this location to the ambulance Case Study (cont’d) • What is the basic disturbance in blood chemistry that can cause respiratory distress? • The patient's dyspnea points to a problem with what body system? • What precautions for your safety should you take? Case Study (cont’d) • Primary Assessment Findings – Patient responsive to verbal stimuli, A&Ox3 – Airway patent, no foreign bodies or fluid – No objective indications of dyspnea present, patient speaks in full sentences Case Study (cont’d) • Primary Assessment Findings – Respiratory rate is 22 times/minute – Peripheral pulse is present, skin is warm and dry Case Study (cont’d) • Is this patient a high or low priority? Why? • What care should be provided immediately? • What information must the body's chemoreceptors be telling the brainstem in order for the respirations to be rapid? Case Study (cont’d) • Medical History – Patient has a history of high blood pressure and “clots in my lungs” • Medications – “I take a blood pressure reducer. It's in my travel bag in my car” • Allergies – Aspirin Case Study (cont’d) • Pertinent Secondary Assessment Findings – Pupils reactive to light, airway patent – Breath sounds clear bilaterally with no accessory muscle use – Pulse oximeter reads 94% on room air Case Study (cont’d) • Pertinent Secondary Assessment Findings – Muscle tone is noted to all extremities – Patient denies any history of trauma – Skin normal – B/P 160/88, Pulse 108, Respirations 22 Case Study (cont’d) • En route to the hospital, the patient states that he was driving to his daughter's home, and that he'd been driving for 11 hours straight, stopping only for fuel. • How might this information be beneficial to understanding the patient's presentation? Case Study (cont’d) • Will you change your treatment based on information you have now learned? • Why is the patient's enhanced ventilation effort not really helping his oxygenation status? Case Study (cont’d) • Care provided: – High-flow oxygen via nonrebreather mask – Place the patient in a position of comfort – Initiate Paramedic intercept prior to departure or en route – Verbally reassure patient en route and provide reassessment Case Study (cont’d) • Explain how oxygen therapy may help improve the patient's condition. • Given this patient's presentation, medical history, and physical exam findings, is he likely using the hypercapnic or hypoxic drive to control respirations? Summary • Consistent with other chapters in this section, understanding the cellular level of functioning will assist the Advanced EMT not only in interpreting the patient's problem, but also managing it more efficiently. • If the cells are not being provided oxygen delivery and carbon dioxide removal, cells will die and the patient can easily die.