Acute Pain - Health Education East Midlands VLE (Moodle)

Principles of Acute Pain
Management
29.9.10
Rik Kapila
What this talk isn’t….
A pharmacology lecture
A physiology lecture
Comprehensive
What this talk is ( I hope!)….
An overview
Relevant
Enlightening
Interesting
An opportunity
What is pain?
“An unpleasant sensory and emotional experience arising from actual or potential tissue damage or described in terms of such damage”.
International Association for the Study of Pain
Perhaps more usefully…
“whatever the experiencing person says it is, existing whenever he says it does."
Margo McCaffrey 1968
Epictetus (55-135 A.D)
‘It is not death or pain that is to be dreaded but the fear of pain or death’
Lance Armstrong (1971- present)
‘pain is temporary – quitting lasts forever’
Saint Augustine of Hippo (354-430)
‘the greatest evil is physical pain’
Does pain matter?
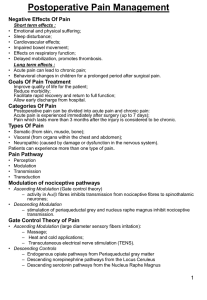
Cardiovascular
Tachycardia
Hypertension
Increased myocardial oxygen consumption
Myocardial ischaemia
Respiratory
Decreased lung volume
Atelectasis
Decreased cough
Sputum retention
Infection
Hypoxia
Gastrointestinal
Decreased gastric motility
Decreased bowel motility
Ileus
Genitourinary
Urinary retention
Metabolic
Increased catabolic hormones
–
–
–
Cortisol
Glucagon
Growth hormone
Reduced anabolic hormones
– Insulin
– Testosterone
Psychological
Anxiety
Fear
Sleep disturbance
Depression
Distressing for patient, family and staff
Chronic Pain after Surgery
Not fully understood
Worse after some surgery than others
Aggressive acute management may reduce incidence of chronic problems
But more of that later….
This is why pain matters
Endogenous morphine
1975 endorphin enkephalin
Dynorphin
synthesised in pituitary
Receptors in the peri-aqueductal gray matter
Endogenous morphine
Responsible for “hedonistic tone”
Increase descending inhibition in spinal cord
Increased release in:
–
–
–
–
– happiness touch / massage sex exercise hypnosis / relaxation
– placebo effect -anticipation of the above
Endogenous morphine
Increased release in:
–
–
–
–
–
– happiness
Increase descending inhibition in spinal cord touch / massage sex exercise hypnosis / relaxation
– placebo effect -anticipation of the above
Reversed by naloxone
How does this link in with the anatomy?
On the way up…
A δ - fast - instant reaction
C - slow - throbbing after-pains / chronic pain
A β - non-pain but inhibit Aδ and C when stimulated
Rubbing / massage / TENS
Local anaesthetics - block
NSAIDS and ketamine - modulate
Pain to cortex via spino-thalamic tract
How does this link in with the anatomy?
In the central processor…
Augment the endorphin system
placebo
opioids
Psychological
Self-hypnosis / relaxation
How does this link in with the anatomy?
On the way down…
Noradrenergic pathways - inhibitory
adrenaline in spinals ?
Serotonin pathways facilitate
Block with ondansetron !
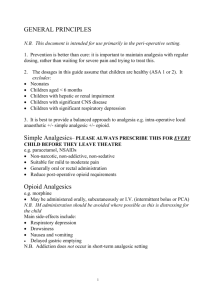
How can we manage pain?
Multimodal
Multi disciplinary
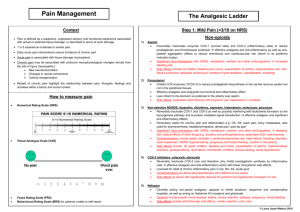
Analgesic ladder
WHO
Simple analgesics first
Moderate opioids next
Strong opioids last
Paracetamol
Is fantastic!
Paracetamol
Paracetamol in acute postoperative pain
Clinical bottom line
Paracetamol is an effective analgesic.
A single dose of 1000 mg paracetamol had an NNT of 3.8 (3.4-4.4) for at least 50% pain relief over 4-6 hours in patients with moderate or severe pain compared with placebo based on information from
2,759 patients.
Paracetamol is not associated with increased adverse effects in single dose administration.
NSAIDS
Non-selective eg. Diclofenac, ibuprofen
Selective eg. Parecoxib, celecoxib
NSAIDS
Good
–
–
– Part of multimodal analgesia
Bone pain
Opioid sparing
Bad
–
–
–
–
Gastric
Renal
Asthma
Bleeding
GRAB
Codeine
Oral codeine in acute postoperative pain
Clinical bottom line:
Codeine 60 mg orally is not an effective analgesic for postoperative pain.
A 60 mg oral dose of codeine had an NNT of
16.7 (11-48) for at least 50% pain relief over
4 to 6 hours compared with placebo in pain of moderate to severe intensity.
Tramadol
Oral tramadol in postoperative pain
Clinical bottom line: Tramadol is an effective analgesic in postoperative pain. A single 100 mg oral dose of tramadol is equivalent to 1000 mg paracetamol. A dose of 100 mg had an
NNT of 4.6 (3.6-6.4) for at least 50% pain relief over 4-6 hours in patients with moderate to severe pain compared with placebo.
At doses of 50 and 100 mg incidence of adverse effects
(headache, nausea, vomiting, dizziness, somnolence) was similar to comparator drugs. In dental trials there was increased incidence of vomiting, nausea, dizziness and somnolence.
Morphine
The standard against which others are measured
Effective
May have side effects
Cheap
Oxycodone
Synthetic opioid
Developed in 1916 in Germany
Why use oxycodone?
Subjectively
–
–
Better tolerated
Feel less ‘weird’
Objectively
– Less hallucinations
Lets use it all the time!
Expensive
–
–
MST 20mg
Oxycontin 10mg
Better but not perfect
18p
47p
Still have side effects
Second line to morphine in cancer pain
– Br J Cancer 84(5);587-593
Morphine – Oxycodone relationship
MST (regular) Oxycodone MR (reg)
– Oxycontin
Oral morphine solution
(prn)
Oxycodone IR (prn)
– Oxynorm
20mg orally
10mg orally
How do regular and PRN work together
Regular Px?
Having lots of prn?
Is the prn dose enough?
Increase the regular dose
Opioid problems
Respiratory depression
Sedation
Constipation
Nausea and vomiting
Ileus
Urinary retention
Etc, etc, etc…..
Nausea and vomiting
All of them can cause it
Morphine is especially good at it
Changing analgesic may help
If someone is vomiting give the antiemetics intravenously!
Itching
Opioids can cause itching
Especially with neuraxial administration
Difficult to treat
Ondansetron can help
Low dose naloxone can help
Chlorpheniramine less so
Oramorph
City Campus
–
–
–
– Single nurse administration
Used lots and lots
Predictable
Oral opioid of choice
Queens Campus
–
–
–
–
2 nurses needed
Used much less
Alternatives used instead
Sevredol, tramadol, DHC
Why?
I have absolutely no idea!
Abuse and addiction
Its is a potential problem
Don’t let that stop you treating pain
Routes of administration
Oral
Subcut
Intramuscular
Intravenous
Transdermal
Epidural
Intrathecal
Local Anaesthetics
Lots of uses
But you may see them cropping up in the following places:
Epidurals
Used in surgical patients
The significance of the little girl?
Spinals
Intra and post op analgesia
Can have opiate added to them
Need to watch for respiratory depression
Should have PCA obs even if they don’t have a PCA
But it still hurts…..
Take a critical look at the drug card
What have they got?
Regular or PRN?
How much?
How often?
Are they actually taking it?
Is the route appropriate?
Pain Team
Help on many levels if you have a pain challenge:
– IVDU
– Acute on chronic pain
– Pregnancy
– Neuropathic pain
Call for advice
How can we do it better?
Identify
Regular assessment
At rest is not enough
Can they cough?
Can they deep breathe?
It is easy to be comfortable lying still!
Respond
‘An hour of pain is as long as a day of pleasure’
Anon
Be careful not to be prejudiced
– Acad Emerg Med 2006;13:140-146
Educate
Patients
Nurses
Surgeons
Anaesthetists
Kiss-it-Better Hospital
Don’t forget the psychological side
Don’t forget that time and some physical contact can make a huge difference
Acknowledge the problem and support the patient
And finally….
“Pain makes man think.
Thought makes man wise
Wisdom makes life endurable .”
(John Patrick 1905-1995)
Pumps and Stuff
PCA - City
Omnifuse
Clinician code 66643
Just imagine you were texting OMNIFUSE!
PCA - QMC
Graseby
No code
Need a key
Can’t do clinician bolus
But Omnifuse should be coming at some point this year
Epidurals (non-obstetric)
Gemstar
Yellow livery
Code 6546
Paravertebrals
Gemstar
Grey livery
Code 1970
Think of Mr Catton!
Wound infusions
Nerve infusion analgesia
The End