Case:
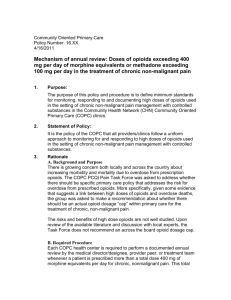
advertisement

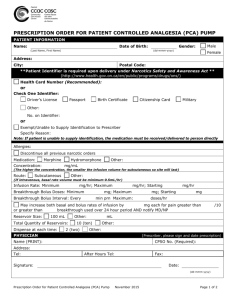
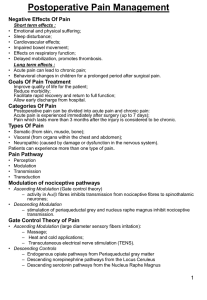
Mini Cases: Pain Management Do the following conversions: • 90 mg morphine PO = • 45 mg hydromorphone IV = • 120 mg oxymorphone PO = • 100 mg morphine PO/day = • 100 mg morphine PO/day = mg Hydromorphone PO mg Oxycodone PO mg Morphine IV mcg/hr Fentanyl TD patch mcg/hr Fentanyl IV Case 1: You get a call from a physician resident on a general medicine service. He says, “I need to know what dose of Duragesic® to start for this patient. She has been using Percocet® 5 mg, about 12 tablets a day for the last week while she was here. She is going home tomorrow. What dose should I write?” Case 2: One of the hospitalists working at your hospital is calling for your help with an IV to PO conversion for JJ. For the last 6 days, JJ has been receiving hydromorphone IV 1.5 mg/hr continuously with 2 mg q15 minutes prn. What questions do you have for the physician before you can help? What dose of Oxycodone SR (OxyContin®) would you recommend? What would you recommend for breakthrough pain? Case 3: AN is a 26 yr old female with chronic pain related to Sickle Cell disease. She has a PCP that writes for Morphine SR (MSContin®) 60 mg TID and oxycodone IR 15 mg TID prn. She presents to the ED today complaining of increasing pain (9/10) consistent with her typical crisis pain. Thirty minutes after receiving hydromorphone IV (Dilaudid®) 1 mg, the patient still rates her pain at 9/10. The RN wants to know if it is okay to give her more pain medication at this time. What dose do you recommend? AN has been in the hospital for 7 days, and is preparing for discharge. In the last 24 hours, she has used Morphine SR (MSContin®) 60 mg TID, hydromorphone 4 mg IVP x 2 doses, and oxycodone IR 60 mg x 4 doses. What dose of Morphine SR (MSContin®) should she be discharged on? 1 Quick Points: Pain Management Questions to ask: What is the source of pain? o Is this acute pain? o Has the pain changed recently/ will the pain change soon? Is this dose controlling pain? (i.e. what is the pain score?) Are there side effects? (most importantly, sedation or respiratory depression) Scheduled Opioids: o Options for scheduled opioids include, sustained release oral or transdermal formulations, aroundthe-clock immediate release formulations, continuous opioid infusions. o Reserve scheduled opioids for chronic, persistent pain. Breakthrough dosing: 10-20% of the schedule daily dose of opioids o Example: For a patient using Morphine SR 100 mg po q8h, the appropriate dose for breakthrough pain would be Morphine IR 30-60 mg po prn pain. For acute or breakthrough pain, opioids can be safely redosed after they reach peak effect. Titration: For uncontrolled pain: o Increase 25-50% for mild to moderate pain o Increase 50-100% for moderate to severe pain o EXCEPTION: Generally, do not recommend more than a 50% increase in methadone at any one time. For patients with opioid-induced sedation or neurotoxicity: Decrease dose 25-50% Switching opioids: Use equianalgesic doses. Reduce calculated dose 0-50% to account for incomplete cross tolerance and variations in individual responses. o General guideline for reduction of calculated dose: 0%- continues to have moderate to severe pain, no sedation present 25%- continues to have mild to moderate pain, no sedation present 50%- has no pain to mild pain OR sedation present with any pain score IMPORTANT NOTE: All opioid dose changes should be made on a percentage basis, not mg. It is more dangerous to increase a patient’s dose from Morphine IV 1 mg/hr to Morphine IV 3 mg/hr (200% increase) than to increase from Morphine IV 30 mg/hr to Morphine IV 60 mg/hr (100% increase). Opioids Analgesic Classes • Phenanthranes – Morphine – Codeine – Hydromorphone – Oxycodone – Hydrocodone • Phenylpiperidines – Meperidine – Fentanyl • Diphenylheptanes – Methadone 2