February 2015 - Devon Sessional GPs
advertisement
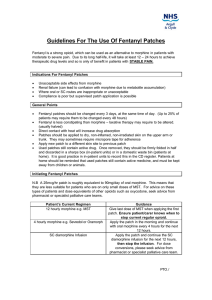
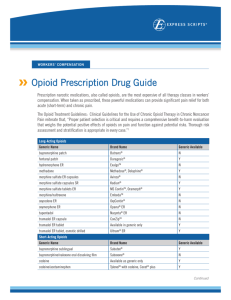
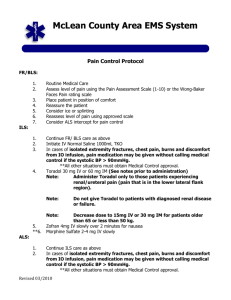
Minutes of the Exeter Sessional GPs Group Darts Farm – 3 February 2015 The meeting was kindly sponsored by: Grunenthal Kate Fuller Ashfield Isaac Chan Jeremy Stevens Attendance: 31 members Welcome: Dr Ross Hemingway opened the meeting and thanked the reps for sponsoring. He reminded members to sign the attendance register which is essential for the reps who fund the meetings. Ross mentioned two longer term locum opportunities, both on the website – Chiddenbrook in Crediton from April to October and St Leonards in July. Each rep gave a short talk and Ross introduced and thanked the speaker Dr Becky Baines – Consultant in Palliative medicine for Hospiscare and RDE. Clinical meeting Dr Becky Baines Consultant in Palliative medicine – Hospiscare and RDE Palliative Medicine Update 1. Prescribing Issues Immediate release fentanyl – place for use for incident pain as it has onset in only 6-10 minutes and does not tend to accumulate so stops working quickly too. Can use it for bone pain on weight bearing, pain on being moved / turned, as absorbed through buccal mucosa or nasal spray can use if absorption problems e.g. bowel obstruction. It is expensive though – e.g. £5 per tablet. Ensure treatment with NSAID, radiotherapy, steroid, bisphosphonate as appropriate to spare opioid. It is worth trying oramorph and immediate release oxycodone first. Neuropathic pain – important to spot it – descriptions include pins and needles, stabbing, electric shock, numb, shooting, throbbing, burning. Gabapentin for neuropathic pain cheaper than pregabalin and easier to titrate (100mg at night 1st day, 100mg bd then 100mg tds over 3 days or if desperate then tds from day 1; can go up to 3,600mg per day in divided doses). Amitriptyline – needs to be 30-50mg for effective relief – start low and work up, taking at 5pm can avoid hangover effect. Lidocaine patches – expensive but sometimes useful, applied to site of worst pain, usually after a failed trial of gabapentin (+/- amitriptyline). Use maximum of 3 patches at a time – due to cardiotoxicity. Not an instant benefit, high placebo effect. Use on for 12 hours and off for 12 hours – the on time often at night as that is when the pain is most troubling. 2 New brands of old opioids – less expensive so use encouraged. Zomorph less expensive than MST but no 5mg or 15mg unit dose, can sprinkle capsule contents on food or give via Peg. Longtec rather than Oxycontin and Shortec rather than Oxynorm are both less expensive. Matrifen patch less expensive than Durogesic. Renal failure – patients withdrawing from dialysis or opting for no dialysis. Buprenorphine ok to use. Fentanyl patches are safest but need stable pain and 12mcg /hr is lowest dose and equivalent to 40mg per day of oral morphine. Oxycodone – long acting and immediate acting both well tolerated – start low and watch for side effects. Sub lingual fentanyl works well for shortness of breath due to pulmonary oedema. Renal end of life – fentanyl safest in CKD 4-5 – is best in syringe driver as short half-life and prn injections only last 2 hours. Starting stat dose 25mcg and syringe driver start at 100-200mcg over 24 hours. Ampoules are 50mcg/ml so volume too high to increase dose a lot and so may need alfentanil for cancer patients with significant pain who go into renal failure. Oxycodone can be better in many cases. Itch – emollients – doublebase, aveeno are good. Ondansetron can be used and if it works then convert to sertraline. Look for underlying causes of itch. Joined up care Just in case bag – a lot of work to get these in place as multiple organisations involved. The bag fully stocked costs approx. £25. In the first two years 1510 bags used (£37,750) but estimated to have saved 121 admissions which would have cost about £350,000. Plus patients like them – gives peace of mind. Future plan to have pre-printed prescription – except for the diamorphine which needs individual dosing. TEP form – now on version 10. Again needed agreement from a lot of stakeholders. Particularly following the case where it was clarified in court that resuscitation decisions cannot be made without patient consent unless actively discussing would do harm to patient, it is important to document discussions about resuscitation. Often best to start by talking about the illness and what can medicine offer – what are the realistic benefits. Electronic messages – on Adastra Gold standards framework – used in community for a long time. Is being introduced in to hospitals. Marie Curie night sitters – unfortunately night sitting nurses difficult to get though – they can give SC injections which would be an advantage. There is a number for palliative patients to use out of hours to bypass 111. If they do get 111 then if there is an electronic message they get passed though rapidly. What went wrong with LCP? – it got used in other settings such as neurology when end of life is less predictable than in cancer. Pathway was being used and not communicated with patient and family about what it meant and why it was in place. It is important to plan with JIC bag, TEP form etc and discuss what the patient wants. Some NEW Devon CCG documents in development – but long, supposed to be initiated by GP so tends not to happen and not used in community hospitals. It is important to think of the principles and document everything. 3 Planning for your future care booklet (Pony booklet because of photo on cover) – covers advance care planning. Other issues Fluids – discuss giving or not giving. IV fluids can be painful to give. Discuss with patient / family – body shutting down, fluids can often get to wrong place – e.g. pulmonary oedema. Can give SC if patient / family are adamant. Opioid conversion charts useful – in JIC bag, on-line. Don’t remove fentanyl patch at end of life – add extra medications to syringe driver, calculate dose by converting fentanyl to oral morphine equivalent and then give increment in driver. Communicate. Use the word “dying”. Crises at end of life – above all keep calm and establish presence – arterial bleed – dark towels, seizures – midazolam, falls and fractures, choking, severe shortness of breath – fan can help, panic by patient or carer. Diamorphine is drug of choice in driver - cannot write up driver pre emptively though. A few equivalences – oral morphine: sc diamorphine 3:1; oral morphine: sc morphine 2:1; oral oxycodone: sc oxycodone 2:1. Hospiscare ward – 01392 688044 – doctor available 24 hours. Hospice has 12 beds but 700 patients. Take admissions 24 hours, can do short burst IV fluids or antibiotics but not if that is the primary need. Can do ascites drains – although often not as need ultrasound, do not do pleural aspirations on site. Criteria for admission – complexity and crisis. Future ESGPG Meetings 3rd March 2015 – Elderly Care Update – Dr Anthony Helmsley Meeting time Please note that the meetings are now scheduled to start at 7pm with the guest speaker planned to commence at 7.30pm. Committee Contacts Dr Ross Hemingway (chair) rosshemingway@me.com Dr Laura Davies (website co-ordinator) ledavies@doctors.org.uk Dr Sarah Hemingway (funding and educational co-ordinator) sarah.hemingway@me.com Dr Anna Beazley (treasurer and educational co-ordinator) abeazley22@outlook.com Dr Kathryn Shore (minutes’ secretary) kathrynshore@btinternet.com